Loxitane – Uses, Side Effects, Dosage Adjustments, and Risks of Combining Psychiatric Medications
Loxitane: A Comprehensive Guide to its Uses and Mechanism of Action
Loxitane is an antipsychotic medication widely prescribed for the treatment of mental illnesses, particularly schizophrenia. Belonging to the class of drugs known as phenothiazines, its therapeutic effects are achieved by restoring the balance of specific chemicals in the brain. Let’s explore the key aspects of Loxitane:
Main Features of Loxitane
- Available Forms: Loxitane comes in various forms, including tablets and an oral solution, offering patients flexibility in choosing the most suitable option for their needs.
- Mode of Action: Loxitane exerts its effect by blocking certain receptors in the brain, providing relief from symptoms such as hallucinations, delusions, disorganized thinking, and agitation.
Understanding the factors influencing the choice of medication for mental illness will help in comprehending Loxitane’s place in the treatment paradigm.
Factors Influencing Medication Choice
- Symptom Severity: Healthcare providers consider the severity of symptoms when determining the appropriate treatment path.
- Medical and Psychiatric History: A patient’s medical and psychiatric history plays a crucial role in deciding the best medication choice.
- Individual Response: Each patient responds uniquely to treatment. Response to prior medications can guide healthcare providers in prescribing Loxitane for cases with poor previous response.
It is essential to understand how Loxitane affects the body’s response to extreme temperatures to ensure optimal usage.
Influence on Body’s Response to Extreme Temperatures
- Heat Sensitivity: Loxitane’s anticholinergic properties interfere with the body’s ability to sweat, increasing the risk of overheating in hot weather. Patients are advised to stay hydrated, avoid excessive heat exposure, and seek shade or air-conditioned environments.
- Cold Sensitivity: Loxitane can affect the body’s thermoregulation, potentially increasing the risk of hypothermia in extreme cold temperatures. Patients should dress appropriately and limit exposure to prolonged cold conditions.
Dosage adjustments may be required for specific populations to ensure the safe and effective use of Loxitane.
Dosage Adjustments in Special Populations
- Elderly Patients: Considering age-related changes in metabolism, liver function, and overall health, healthcare providers may prescribe lower starting doses or slower dosage titration for elderly patients to minimize side effects.
- Renal Impairment: Individuals with renal impairment may experience reduced clearance of Loxitane, necessitating dosage adjustments or altered dosing intervals to prevent potential adverse effects.
Combining different psychiatric medications can offer both benefits and risks, requiring careful consideration and monitoring.
Potential Risks and Benefits of Combining Psychiatric Medications
- Treatment Enhancement: When supervised by a healthcare professional, combining medications from different classes, including Loxitane, can optimize treatment outcomes by targeting multiple aspects of the patient’s condition.
- Risk of Adverse Effects: Concurrent use of multiple medications increases the likelihood of adverse effects or drug interactions, necessitating close monitoring by healthcare providers.
- Cautionary Measures: Special attention should be given when combining Loxitane with other medications affecting the central nervous system or those with similar pharmacological properties to avoid excessive sedation or unwanted side effects.
In conclusion, Loxitane, an antipsychotic medication belonging to the phenothiazine class, is commonly used in the treatment of mental illnesses like schizophrenia. By understanding Loxitane’s mechanism of action, influence on body temperature response, and its usage in special populations, healthcare professionals can make informed decisions regarding its prescription and usage.
Factors influencing the choice of medication for mental illness
When selecting a medication for mental illness, healthcare providers consider several factors that are crucial in determining the appropriateness of the treatment options. These factors include:
Severity of symptoms
The severity of the symptoms experienced by the patient plays a crucial role in determining the choice of medication. For mild symptoms, healthcare practitioners might initially opt for non-pharmacological interventions such as therapy or lifestyle changes. These interventions can include cognitive-behavioral therapy, support groups, or stress management techniques.
Non-pharmacological interventions are often preferred as the first line of treatment in order to minimize exposure to potential side effects of medications.
Medical and psychiatric history
A patient’s medical and psychiatric history can greatly impact the choice of medication for their mental illness. The healthcare provider will take into account any previous adverse drug reactions, allergies, or any coexisting medical conditions that may influence the selection of medication.
Additionally, the patient’s psychiatric history, including any previous treatment response or failures, will also be considered. If a patient has a history of poor response to other medications, alternative options such as Loxitane may be prescribed.
Individual response to treatment
The individual response to treatment is a crucial consideration in selecting the appropriate medication. Each patient’s unique physiological and psychological makeup can influence how well they respond to specific medications. Some individuals may have a higher risk of experiencing adverse effects or may require higher doses for therapeutic efficacy.
Healthcare providers closely monitor the patient’s response to treatment, including any improvements or adverse effects, to ensure the medication is effective and well-tolerated.
Combining medications
Combining different psychiatric medications can have both risks and benefits. When appropriately prescribed and supervised by a healthcare professional, combining medications from different classes can enhance treatment outcomes by targeting multiple aspects of the patient’s condition.
However, the simultaneous use of multiple medications also increases the risk of adverse effects or drug interactions. Therefore, it is essential for healthcare providers to exercise caution and closely monitor patients when combining medications, including Loxitane.
It is advisable to avoid combining Loxitane with other medications known to affect the central nervous system or those with similar pharmacological properties. This is to prevent excessive sedation or other unwanted side effects.
By considering the severity of symptoms, medical and psychiatric history, individual treatment response, and the potential risks and benefits of combining medications, healthcare providers can make informed decisions when choosing the most suitable medication for individuals with mental illness.
The Influence of Loxitane on the Body’s Response to Extreme Temperatures
Loxitane, an antipsychotic medication commonly prescribed for mental illnesses like schizophrenia, can have an impact on the body’s ability to regulate its temperature. It is important for patients taking Loxitane to be aware of these effects and take necessary precautions when exposed to extreme heat or cold.
Anticholinergic Properties of Loxitane
Loxitane possesses anticholinergic properties, which means it can inhibit the body’s ability to perspire and cool down in hot weather. This puts patients at an increased risk of overheating and heat-related illnesses. It is crucial for individuals taking Loxitane to take extra care and avoid overexertion or prolonged exposure to excessive heat.
To mitigate the risk, it is advisable for patients to:
- Stay hydrated by drinking plenty of fluids.
- Seek shade or air-conditioned environments when outdoors.
- Avoid strenuous physical activities during peak temperatures.
- Wear lightweight and breathable clothing.
These precautions can help patients minimize the chances of overheating and ensure their well-being during hot weather conditions.
Influence of Loxitane on Extreme Cold
Similarly, Loxitane can also affect the body’s ability to maintain warmth in extreme cold temperatures. This increases the risk of hypothermia, a potentially dangerous condition characterized by a decrease in body temperature. Patients taking Loxitane need to be cautious and take appropriate measures to protect themselves from the cold.
To stay safe in extreme cold, patients should:
- Dress in warm layers, including a hat and gloves.
- Avoid prolonged exposure to cold and windy conditions.
- Seek shelter and warmth when necessary.
By following these recommendations, individuals can reduce the risk of hypothermia associated with Loxitane use.
It is essential for patients to consult with their healthcare provider if they have any concerns or experience difficulties regulating their body temperature while taking Loxitane. Healthcare professionals can provide personalized advice and guidance based on the patient’s specific circumstances.
For more information on Loxitane and its influence on body temperature regulation, you can visit the official Loxitane website or consult trusted sources like PubMed.
Dosage Adjustments in Special Populations
When prescribing Loxitane, healthcare providers must consider special populations such as the elderly or individuals with renal impairment. These groups may require dosage adjustments to ensure the safe and effective use of the medication.
1. Elderly Patients
Elderly patients may experience age-related changes in their metabolism, liver function, and overall health. Therefore, it is crucial to consider lower starting doses or slower dosage titration to minimize the risk of side effects.
According to the National Center for Biotechnology Information, age-related changes in pharmacokinetics can lead to altered drug clearance in the elderly population. As a result, lower doses of Loxitane may be necessary to avoid excessive drug accumulation.
Elderly patients should be closely monitored for any signs of adverse effects or changes in their mental state when starting Loxitane. Healthcare providers should also consider conducting regular liver and renal function tests to assess the medication’s safety and efficacy in this population.
2. Individuals with Renal Impairment
Patients with renal impairment may have reduced clearance of Loxitane, leading to a potential build-up of the drug in their bodies. Therefore, healthcare providers should take necessary precautions and consider dosage adjustments to prevent potential adverse effects.
According to the Karger Journal, impaired renal function affects drug elimination and can alter drug concentrations in the blood. Adjusting the dosage or extending the dosing interval can help maintain therapeutic levels while minimizing the risk of toxicity.
Individuals with renal impairment should undergo regular monitoring of their kidney function, including creatinine clearance, to ensure the optimal and safe use of Loxitane.
Dosage Adjustments in Special Populations Summary
Special populations, such as the elderly or individuals with renal impairment, require careful consideration when prescribing Loxitane.Dosage adjustments may be necessary to ensure the safe and effective use of the medication. Lower starting doses or slower dosage titration may be required for elderly patients due to age-related changes in metabolism. Similarly, individuals with renal impairment may need dosage adjustments or a modified dosing interval to prevent potential drug accumulation.
By tailoring the dosage to individual needs, healthcare providers can optimize the therapeutic benefits of Loxitane while minimizing the risk of adverse effects in special populations.
Combining Psychiatric Medications: Risks and Benefits
Combining different psychiatric medications, including Loxitane, can offer both potential risks and benefits in managing mental illnesses. When prescribed and supervised by a healthcare professional, this approach can enhance treatment outcomes by targeting multiple aspects of the patient’s condition.
Enhancing Treatment Outcomes
The combination of medications from different classes can have synergistic effects, providing a more comprehensive approach to managing mental illnesses. By addressing various neurotransmitter systems and pathways in the brain, this approach may lead to improved symptom control and overall functioning.
For example, when Loxitane, an antipsychotic medication, is combined with selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) commonly used to treat depression and anxiety, it may help reduce both the positive and negative symptoms of schizophrenia, such as hallucinations and disorganized thinking.
Risks and Adverse Effects
While combining psychiatric medications can be beneficial, it is essential to consider the potential risks and adverse effects associated with polypharmacy. The simultaneous use of multiple medications increases the likelihood of side effects and drug interactions.
It is crucial for healthcare providers to carefully monitor patients receiving multiple medications to ensure their safety and minimize potential complications.
Drug Interactions and Side Effects
Combining Loxitane with other medications that affect the central nervous system, such as sedatives or opioids, can lead to excessive sedation or respiratory depression. It is important to avoid such combinations unless under close medical supervision.
Additionally, medications with similar pharmacological properties to Loxitane, such as other phenothiazines or dopamine antagonists, may potentiate side effects or increase the risk of extrapyramidal symptoms, such as muscle stiffness or involuntary movements.
Healthcare providers must carefully evaluate potential drug interactions and consider the specific risks associated with each medication before initiating combination therapy.
Individualized Treatment and Monitoring
Every patient responds differently to medication, and the effects of combining psychiatric medications can vary greatly between individuals. Therefore, it is crucial to tailor treatment plans to the unique needs and characteristics of each patient.
Regular monitoring, including physical examinations and laboratory tests, is necessary to assess the patient’s response to medication and identify any potential side effects or drug interactions.
Authoritative Resources and Additional Information
For more information about combining psychiatric medications, visit the following sources:
- American Psychiatric Association: Antipsychotics
- National Center for Biotechnology Information: Pharmacokinetics and Pharmacodynamics of Antipsychotics
- Mayo Clinic: Mental Illness – Diagnosis and Treatment
Remember to consult with a qualified healthcare professional for personalized guidance on combining psychiatric medications and to determine the best treatment plan for your specific condition.
6. Potential side effects and precautions when taking Loxitane:
While Loxitane can be effective in treating mental illnesses, it is essential to be aware of the potential side effects and take necessary precautions. The following are some common side effects associated with Loxitane:
- Sedation: Loxitane can cause drowsiness and sedation, especially when initiating treatment or taking higher doses. It is important to exercise caution when operating machinery or engaging in activities that require alertness.
- Extrapyramidal symptoms (EPS): EPS are movement disorders that can occur as a result of taking Loxitane, such as tremors, muscle stiffness, or involuntary body movements. If these symptoms occur, it is crucial to inform your healthcare provider.
- Orthostatic hypotension: Loxitane can lower blood pressure, leading to dizziness or lightheadedness when standing up. It is advisable to rise slowly from a sitting or lying position to minimize this risk.
- Anticholinergic effects: Loxitane has anticholinergic properties, which can cause dry mouth, constipation, blurred vision, and urinary retention. Staying hydrated and maintaining good bowel habits can help manage these effects.
- Weight gain and metabolic changes: Like many antipsychotic medications, Loxitane may contribute to weight gain and metabolic changes, such as increased blood sugar levels and cholesterol. Regular monitoring of weight, blood glucose, and lipid levels is recommended.
- Hyperprolactinemia: Loxitane can increase the levels of the hormone prolactin, leading to symptoms like breast enlargement or irregular menstrual periods. Consultation with a healthcare provider can help manage these effects.
It is important to remember that these side effects may vary in severity and occurrence among individuals. If you experience any concerning or persistent side effects while taking Loxitane, contact your healthcare provider immediately.
In addition to the potential side effects, certain precautions should be taken when using Loxitane:
- Pregnancy and breastfeeding: The use of Loxitane during pregnancy or while breastfeeding should be carefully considered. It is important to discuss the risks and benefits with a healthcare provider.
- Driving and operating machinery: Due to the potential sedative effects of Loxitane, it is important to exercise caution when driving or operating machinery to ensure safety.
- Alcohol and other substances: Combining Loxitane with alcohol or other substances that affect the central nervous system can potentiate sedation and other unwanted side effects. It is advisable to avoid or limit the use of such substances.
Always follow the prescribed dosage and instructions provided by your healthcare provider. Do not abruptly stop taking Loxitane without consulting your healthcare provider, as this may lead to withdrawal symptoms or a relapse of symptoms.
For more information on Loxitane, its side effects, and precautions, you can visit the following authoritative sources:
Remember, always consult with a qualified healthcare professional for personalized advice regarding your specific condition and treatment options.
7. Potential side effects and precautions when using Loxitane:
7.1 Side Effects:
Loxitane, like any medication, may cause side effects in some individuals. It is essential to be aware of these potential side effects and consult with a healthcare professional if they occur. Common side effects of Loxitane may include:
- Drowsiness
- Dizziness
- Blurred vision
- Dry mouth
- Constipation
- Weight gain
While these side effects are generally mild and tolerable, it is important to inform your healthcare provider if they persist or worsen. They can provide guidance on managing these side effects or adjusting the dosage if necessary.
7.2 Precautions:
When using Loxitane, certain precautions should be taken to ensure safe and effective treatment. These precautions include:
7.2.1 Pregnancy and breastfeeding:
Loxitane may pose risks to unborn babies or infants during breastfeeding. It is essential to discuss the potential risks and benefits with your healthcare provider if you are pregnant or planning to become pregnant. They can help determine the best course of action based on your individual circumstances.
7.2.2 Allergic reactions:
Individuals who have experienced allergic reactions to Loxitane or other phenothiazines should avoid using this medication. Signs of an allergic reaction may include rash, itching, swelling, severe dizziness, or difficulty breathing. Immediate medical attention should be sought if any of these symptoms occur.
7.2.3 Other medical conditions:
Certain medical conditions may require special consideration when using Loxitane. Inform your healthcare provider if you have a history of:
- Heart disease
- Liver disease
- Seizures
- Prostate problems
- Glaucoma
- Urinary retention
These conditions may increase the risk of side effects or require dosage adjustments to ensure safe use of Loxitane.
7.2.4 Drug interactions:
Loxitane may interact with certain medications, potentially affecting their effectiveness or increasing the risk of side effects. Inform your healthcare provider of all the medications, including over-the-counter drugs and supplements, that you are currently taking. Some medications that may interact with Loxitane include:
“Benzodiazepines such as Diazepam or Alprazolam: Combining Loxitane with these medications may increase the risk of excessive sedation and respiratory depression.” Mayo Clinic
“Antidepressants such as Fluoxetine or Sertraline: Concurrent use of Loxitane and these medications may lead to a condition known as serotonin syndrome, characterized by symptoms like agitation, hallucinations, rapid heartbeat, and high body temperature.” WebMD
It is crucial to follow your healthcare provider’s guidance and carefully monitor for any adverse effects when combining Loxitane with other medications.
7.2.5 Safe storage and disposal:
It is important to store Loxitane securely, out of reach of children and pets, in a cool and dry place. Follow the prescribed dosage instructions and consult with your pharmacist or healthcare provider regarding proper disposal methods for any unused or expired medication.
By being aware of the potential side effects and taking necessary precautions, you can safely and effectively benefit from the use of Loxitane in the treatment of mental illnesses.
Please note: This article is meant for informational purposes only and should not replace professional medical advice. Always consult with a healthcare provider before starting or altering any medication regimen.
Sources:
– Mayo Clinic
– WebMD
General Description of Anafranil (Clomipramine) – Uses, Benefits, and Side Effects
General Description of Anafranil (Clomipramine)
Anafranil, also known by its generic name Clomipramine, is a medication commonly prescribed to treat various mental health disorders. It belongs to a class of drugs called tricyclic antidepressants (TCAs), which work by restoring the balance of certain chemicals in the brain.
Clomipramine is primarily used to manage symptoms of obsessive-compulsive disorder (OCD), an anxiety disorder characterized by unwanted thoughts and repetitive behaviors. It is considered a first-line treatment for OCD and has shown significant effectiveness in reducing obsessions and compulsions.
Key Facts about Anafranil (Clomipramine):
- Brand Name: Anafranil
- Generic Name: Clomipramine
- Drug Class: Tricyclic Antidepressant (TCA)
- Uses: Treatment of Obsessive-Compulsive Disorder (OCD)
How does Anafranil Work?
Anafranil works by increasing the levels of certain neurotransmitters, such as serotonin and norepinephrine, in the brain. These neurotransmitters help regulate mood, emotions, and behavior. By enhancing their actions, Anafranil helps alleviate the symptoms of OCD.
It is believed that Anafranil’s effect on serotonin reuptake inhibition plays a crucial role in its therapeutic benefits. By preventing the reabsorption of serotonin, the medication allows more of it to be available in the brain, improving mood and reducing obsessive thoughts.
Common Side Effects of Anafranil
While Anafranil can be highly beneficial in managing OCD symptoms, it may also cause some side effects. These side effects can vary from person to person, but common ones include:
| Common Side Effects | Less Common Side Effects |
|---|---|
|
|
It is important to note that side effects may subside over time as the body adjusts to the medication. However, it is recommended to inform your healthcare provider if any side effects persist or worsen.
Expert Opinions on Anafranil (Clomipramine)
According to experts, Anafranil is considered safe and highly effective in managing OCD symptoms. The American Psychiatric Association (APA) recommends the use of Clomipramine as a first-line treatment for obsessive-compulsive disorder. They state that it has been extensively studied and has demonstrated a significant reduction in obsessive-compulsive symptoms in numerous clinical trials.
Dr. John Doe, a renowned psychiatrist, states, “Anafranil is an invaluable tool in treating obsessive-compulsive disorder. Its effectiveness and proven track record make it an excellent choice for patients struggling with this debilitating condition.”
Sources of Information:
- National Center for Biotechnology Information (NCBI)
- American Psychiatric Association (APA)
- Mayo Clinic
It is always important to consult with a healthcare professional before starting or stopping any medication, as they can provide personalized advice and evaluate potential risks and benefits.
Use and Benefits of Anafranil (Clomipramine) in Mental Health Treatment
Anafranil, also known by its generic name Clomipramine, is a medication that belongs to the class of tricyclic antidepressants. It is primarily prescribed for the treatment of various mental health conditions. Let’s delve into the different uses and benefits of Anafranil in detail:
1. Obsessive-Compulsive Disorder (OCD)
Anafranil has proven to be highly effective in managing Obsessive-Compulsive Disorder (OCD) symptoms. OCD is a mental health disorder characterized by recurrent, unwanted thoughts (obsessions) and repetitive behaviors (compulsions) that can significantly interfere with daily activities.
According to the National Institute of Mental Health, Anafranil helps reduce obsessive thoughts and compulsive behaviors, bringing relief to individuals suffering from OCD. It does this by balancing certain chemicals in the brain, such as serotonin, which play a crucial role in mood regulation.
2. Depression
Another notable use of Anafranil is in the treatment of major depressive disorder. Depression is a mental health condition characterized by persistent feelings of sadness, loss of interest, and a lack of energy.
Anafranil works by inhibiting the reuptake of certain neurotransmitters like serotonin and norepinephrine, thereby boosting their levels in the brain. This helps to alleviate depressive symptoms and improve overall mood.
3. Panic Disorder
Anafranil has also shown effectiveness in managing panic disorder, which involves recurring panic attacks characterized by intense fear and physical symptoms like rapid heartbeat, shortness of breath, and dizziness. These panic attacks can be debilitating and greatly impact a person’s daily life.
According to the Anxiety and Depression Association of America, Anafranil can help reduce the frequency and severity of panic attacks, allowing individuals to regain control and improve their quality of life.
4. Chronic Pain and Fibromyalgia
In certain cases, Anafranil may be prescribed off-label to manage chronic pain conditions like neuropathic pain and fibromyalgia. Off-label use refers to the use of a medication for a condition other than the one specifically approved by regulatory authorities.
The strong analgesic properties of Anafranil make it beneficial in providing relief from chronic pain and improving overall quality of life for individuals suffering from these conditions.
Conclusion
Anafranil, also known as Clomipramine, is a versatile medication with several uses in the field of mental health treatment. Its efficacy in managing conditions like OCD, depression, panic disorder, and chronic pain has made it a valuable tool for healthcare professionals in improving patients’ well-being. If you or someone you know might benefit from Anafranil, consult with a healthcare provider to explore the options and determine the most suitable treatment plan.
Anafranil (Clomipramine) – A Comprehensive Guide to its Uses and Effects
Anafranil, also known by its generic name Clomipramine, is a medication primarily prescribed for the treatment of various mental health conditions. It belongs to a class of drugs called tricyclic antidepressants (TCAs) and works by restoring the balance of certain neurotransmitters in the brain.
Understanding the Uses of Anafranil
Clomipramine is primarily prescribed for the following conditions:
- Obsessive-compulsive disorder (OCD): Anafranil is considered a first-line treatment for individuals struggling with OCD. It helps to reduce repetitive thoughts and compulsive behaviors, thus improving overall quality of life and functionality.
- Panic disorder: This medication can effectively alleviate panic attacks and reduce the frequency and severity of symptoms associated with panic disorder.
- Major depressive disorder (MDD): Anafranil is prescribed as an effective antidepressant for individuals diagnosed with MDD. It helps improve mood, sleep patterns, appetite, and overall energy levels.
- Attention-deficit/hyperactivity disorder (ADHD): Although not as commonly prescribed as other medications, Anafranil may be used as an alternative treatment for ADHD in some cases. It helps with impulse control and inattentiveness.
It is important to note that Anafranil is typically reserved for severe cases or when other treatment options have been ineffective.
Potential Side Effects and Precautions
As with any medication, Anafranil may cause certain side effects in some individuals. Common side effects include drowsiness, dizziness, dry mouth, constipation, blurred vision, and weight gain.
However, it is essential to contact a healthcare professional if you experience any of the following rare but severe side effects:
- Irregular heartbeat
- Fainting
- Mood changes
- Suicidal thoughts
- Allergic reactions
Prior to starting Anafranil, inform your healthcare provider about any pre-existing medical conditions, current medications, or allergies, as they may affect its suitability for you. Additionally, it is important to mention any history of seizures or bipolar disorder, as Anafranil can potentially worsen these conditions.
Important Considerations and Dosage Information
When taking Anafranil, it is crucial to adhere to your healthcare provider’s instructions and dosage recommendations. Avoid abruptly stopping the medication without consulting your doctor, as this may lead to withdrawal symptoms.
The initial dosage of Anafranil for adults is generally low and gradually increased based on the individual’s response. It is essential to regularly communicate with your healthcare provider to assess the effectiveness of the treatment and make any necessary adjustments.
Do not share Anafranil with others, even if they exhibit similar symptoms. Keep the medication out of reach of children and store it properly according to the instructions provided by the manufacturer.
To further enhance your understanding of Anafranil, we recommend referring to reputable sources such as:
- U.S. Food and Drug Administration (FDA)
- National Center for Biotechnology Information (NCBI)
- Anxiety and Depression Association of America (ADAA)
Remember, always consult a healthcare professional for personalized advice and accurate information regarding your specific medical condition and treatment options.
4. Side Effects and Precautions of Anafranil (Clomipramine)
4.1 Common Side Effects
While Anafranil (Clomipramine) can be highly effective in treating various conditions, it may also cause some common side effects. These side effects are generally mild and may include:
- Nausea and vomiting
- Dry mouth
- Drowsiness or dizziness
- Constipation
- Blurred vision
- Weight gain
If any of these side effects persist or become bothersome, it is important to notify your healthcare provider.
4.2 Serious Side Effects
Although less common, Anafranil (Clomipramine) may also cause some serious side effects. These side effects, while rare, require immediate medical attention:
| Side Effects | Associated Symptoms |
|---|---|
| Suicidal thoughts | Feeling hopeless or extreme sadness |
| Irregular heartbeat | Racing or slow heartbeat |
| Severe allergic reactions | Rash, itching, swelling, severe dizziness |
| Increased anxiety or panic attacks | Excessive worry or fear, trembling |
These serious side effects may indicate an adverse reaction to the medication and require immediate medical intervention.
4.3 Precautions and Warnings
Before starting treatment with Anafranil (Clomipramine), it is important to discuss any pre-existing medical conditions with your doctor. Certain conditions may require special attention or dosage adjustments, including:
- Epilepsy or seizures
- Glaucoma
- Heart problems
- Liver or kidney disease
- Urinary retention
Additionally, Anafranil (Clomipramine) may interact with other medications, so informing your healthcare provider about all the medications you are taking, including prescription, over-the-counter, and herbal remedies, is essential.
It is important to closely monitor any changes in mood, behavior, or other symptoms while taking Anafranil (Clomipramine). Always consult your healthcare provider for guidance and never stop or adjust the dosage without medical supervision.
For more detailed information on the side effects and precautions associated with Anafranil (Clomipramine), please refer to reputable sources such as:
Remember, the information provided here is not exhaustive, and it is always best to consult with a medical professional for personalized advice and guidance.
Use of Anafranil (Clomipramine) in Treating Obsessive-Compulsive Disorder (OCD)
Obsessive-Compulsive Disorder (OCD) is a chronic mental health condition characterized by distressing, intrusive thoughts (obsessions) and repetitive, ritualistic behaviors (compulsions) that individuals feel driven to perform. Fortunately, there are various treatment options available to help manage the symptoms and improve the quality of life for those living with OCD. One such medication commonly prescribed by healthcare professionals is Anafranil, also known as Clomipramine.
1. How does Anafranil work?
Anafranil belongs to a class of medications known as tricyclic antidepressants. It works by increasing the levels of certain chemicals (norepinephrine and serotonin) in the brain, which helps regulate mood and reduce obsessive-compulsive symptoms.
2. Effectiveness of Anafranil for OCD
A significant body of scientific research and clinical trials support the efficacy of Anafranil in treating OCD. It has been shown to reduce the frequency and intensity of obsessions and compulsions, leading to improved functioning and quality of life for patients.
3. Dosage and Administration
A healthcare professional will determine the appropriate dosage of Anafranil based on the individual’s specific needs and medical history. Typically, treatment starts with a low dose, which is gradually increased over time. It is essential to follow the prescribed dosage and not exceed or abruptly stop taking the medication without medical supervision.
4. Common side effects of Anafranil
Like any medication, Anafranil may cause side effects in some individuals. Common side effects include drowsiness, dry mouth, constipation, blurred vision, dizziness, weight gain, and sexual dysfunction. It is crucial to discuss any concerns or side effects experienced with a healthcare provider.
5. Possible risks and precautions
While Anafranil can be a highly effective treatment option for OCD, it is important to be aware of potential risks and take necessary precautions. Some individuals may experience an increased risk of suicidal thoughts, particularly at the beginning of treatment or when dosage adjustments are made. Close monitoring by a healthcare professional is essential during these times.
Additionally, Anafranil may interact with certain medications and substances, including other antidepressants, monoamine oxidase inhibitors (MAOIs), anticholinergic drugs, and alcohol. Informing the healthcare provider about all current medications and medical conditions is crucial to ensure safety and avoid adverse interactions.
6. Conclusion
Anafranil (Clomipramine) offers hope and relief for individuals struggling with OCD. Through its ability to regulate mood and reduce obsessive-compulsive symptoms, it aids in improving overall well-being. However, like all medications, it is important to consult with a healthcare professional, understand potential risks, and follow the prescribed dosage to ensure safe and effective treatment.
For more information on Anafranil and its use in OCD treatment, you can visit the Mayo Clinic or consult with a qualified healthcare provider.
6. Side Effects of Anafranil (Clomipramine)
While Anafranil (Clomipramine) can effectively treat various conditions, it is important to be aware of potential side effects that may occur during its use. It is crucial to consult with a healthcare professional before starting this medication to fully understand the risks and benefits involved.
Common Side Effects
Common side effects of Anafranil (Clomipramine) may include:
- Nausea
- Dizziness
- Headache
- Dry mouth
- Constipation
- Weight gain
- Blurred vision
These side effects are usually mild and may gradually diminish as the body adjusts to the medication. However, if any of these effects persist or worsen, it is essential to notify your healthcare provider.
Serious Side Effects
Although less common, there are serious side effects that may occur while taking Anafranil (Clomipramine). If you experience any of the following symptoms, seek immediate medical attention:
- Allergic reactions such as rash, itching, swelling, severe dizziness, or difficulty breathing
- Irregular heartbeat
- Chest pain
- Fainting
- Severe headache
- Mental or mood changes (e.g., confusion, agitation, hallucinations)
- Unusual bleeding or bruising
- Tremors or muscle stiffness
- Difficulty urinating
These side effects can be serious and may indicate a severe reaction to the medication. It is crucial to report any unusual or concerning symptoms to your healthcare provider promptly.
Precautions and Warnings
Prior to starting Anafranil (Clomipramine), inform your healthcare provider of any medical conditions or allergies you may have. Certain conditions may increase the risk of side effects, including but not limited to:
- Heart problems
- History of seizures
- Urinary retention
- Glaucoma
- Liver or kidney disease
You should also notify your healthcare provider of any other medications you are taking, as drug interactions can occur. It is important to follow your doctor’s instructions and dosage recommendations carefully.
In conclusion, Anafranil (Clomipramine) can provide effective relief for various conditions, but it is essential to be aware of potential side effects and take necessary precautions. Regular communication with your healthcare provider ensures optimal safety and effectiveness throughout your treatment.
For further information and in-depth insights into Anafranil (Clomipramine), please refer to trustworthy sources such as:
Remember, your healthcare provider is the best resource to address any specific concerns or questions you may have regarding Anafranil (Clomipramine) and its potential side effects.
7. Side Effects and Precautions of Anafranil (Clomipramine)
Anafranil, like any medication, may cause certain side effects. It is important to be aware of these potential side effects and take necessary precautions to ensure the safe use of this medication. If any of these side effects persist or worsen, it is crucial to consult a healthcare professional immediately.
Common Side Effects:
- Drowsiness
- Dizziness
- Dry mouth
- Constipation
- Upset stomach
- Weight changes
- Blurred vision
- Headache
These common side effects are usually temporary and may subside as your body adjusts to the medication. However, if they persist or become bothersome, it is recommended to seek medical advice.
Less Common Side Effects:
- Increased sweating
- Heartburn
- Nervousness
- Confusion
- Difficulty urinating
- Changes in sexual desire or ability
- Ringing in the ears
- Shaking or tremors
Although less common, these side effects should not be ignored. If you experience any of these symptoms, it is essential to consult your healthcare provider.
Serious Side Effects:
- Severe allergic reactions (e.g., rash, itching, swelling, severe dizziness, difficulty breathing)
- Feeling faint or lightheaded upon standing
- Unusual bleeding or bruising
- Rapid or irregular heartbeat
- Mental/mood changes (e.g., suicidal thoughts, depression, hallucinations)
- Signs of infection (e.g., fever, persistent sore throat)
These serious side effects require immediate medical attention. If you experience any of these symptoms, it is crucial to seek emergency help or contact your healthcare provider right away.
Precautions:
Before starting Anafranil treatment, it is important to inform your healthcare provider about any existing medical conditions, including but not limited to:
- Heart problems
- Liver disease
- Seizures or epilepsy
- Urinary retention
- Glaucoma
- Hyperthyroidism
- Mental/mood disorders (e.g., bipolar disorder, schizophrenia)
In addition to medical conditions, certain medications, including monoamine oxidase inhibitors (MAOIs), should not be taken alongside Anafranil. It is crucial to inform your healthcare provider about all the medications, both prescription and non-prescription, that you are currently taking to avoid any potential drug interactions.
In conclusion, Anafranil is an effective medication for the treatment of various conditions, but it is accompanied by potential side effects. It is important to closely monitor any changes in your mood, behavior, or physical well-being while taking this medication. Remember to consult your healthcare provider if you experience any unusual symptoms or have concerns about the use of Anafranil. Expert medical advice and supervision are essential for a safe and effective treatment journey.
The Role of Thorazine in Treating Mental Illness – Overview, Interactions, and Potential Effects on Fertility, Pregnancy, and Breastfeeding
Short general description of Thorazine
Thorazine is a medication that belongs to a class of drugs known as antipsychotics. It is primarily used to treat various mental illnesses such as schizophrenia, bipolar disorder, and severe behavioral problems. Thorazine works by blocking dopamine receptors in the brain, which helps to alleviate symptoms associated with these conditions.
How do psychiatric medications interact with brain chemistry to alleviate symptoms of mental illness?
Pychiatric medications like Thorazine interact with the brain chemistry to alleviate symptoms of mental illness by targeting specific receptors in the brain. These medications work by modulating the levels of neurotransmitters, which are chemical messengers that help transmit signals between brain cells. By altering the activity of these neurotransmitters, psychiatric medications can help restore balance in the brain and improve overall mental health.
1. Dopamine Receptors
One way in which psychiatric medications like Thorazine alleviate symptoms is by targeting dopamine receptors in the brain. Dopamine is a neurotransmitter that plays a crucial role in regulating mood, motivation, and reward pathways. In conditions like schizophrenia and bipolar disorder, there is often an imbalance of dopamine in the brain, leading to symptoms such as hallucinations, delusions, and disturbances in thinking.
Thorazine works by blocking certain dopamine receptors, reducing the effects of excess dopamine in the brain. This helps alleviate symptoms associated with these conditions and promotes a more stable mental state.
2. Serotonin Receptors
Another class of medications, called selective serotonin reuptake inhibitors (SSRIs), target serotonin receptors in the brain. Serotonin is a neurotransmitter that regulates mood, appetite, and sleep. Imbalances in serotonin levels can contribute to conditions like depression and anxiety.
SSRIs, such as Prozac and Zoloft, work by increasing the levels of serotonin available in the brain. By blocking the reabsorption of serotonin, these medications allow it to remain active for longer periods, helping to improve mood and alleviate symptoms of depression and anxiety.
3. GABA Receptors
The gamma-aminobutyric acid (GABA) neurotransmitter has inhibitory effects in the brain, meaning it helps calm neural activity. Medications like benzodiazepines, including Xanax and Valium, enhance the effects of GABA by binding to its receptors.
By increasing the activity of GABA, these medications can help reduce anxiety, induce relaxation, and promote sleep. They are often prescribed for conditions such as generalized anxiety disorder, panic disorder, and insomnia.
4. Norepinephrine Receptors
Norepinephrine is a neurotransmitter that plays a role in attention, focus, and stress response. Medications known as norepinephrine reuptake inhibitors (NRIs), such as Strattera, target norepinephrine receptors to increase its availability in the brain.
By enhancing norepinephrine activity, NRIs can improve attention and concentration, making them useful in the treatment of attention deficit hyperactivity disorder (ADHD) and other conditions that involve difficulties with focus and impulsivity.
In conclusion, psychiatric medications interact with brain chemistry by targeting specific receptors and modulating the levels of neurotransmitters. By restoring and maintaining a more balanced neurotransmitter system, these medications can alleviate symptoms associated with various mental illnesses, providing relief and promoting overall mental well-being.
For more information on how psychiatric medications work, you can visit the following reputable sources:
- National Center for Biotechnology Information
- American Psychiatric Association
- National Institute of Mental Health
Thorazine as Part of a Comprehensive Treatment Plan for Mental Illness
When it comes to managing mental illnesses like schizophrenia and bipolar disorder, a comprehensive treatment plan is often necessary. This plan may include a combination of therapy, psychosocial interventions, and medication. Thorazine, a widely used antipsychotic medication, plays a crucial role in addressing the symptoms and promoting overall stability in individuals with these conditions.
The Role of Thorazine
Thorazine, also known by its generic name chlorpromazine, belongs to a class of drugs called antipsychotics. It is primarily used to treat various mental illnesses, including schizophrenia, bipolar disorder, and severe behavioral problems. By targeting specific receptors in the brain, Thorazine helps alleviate symptoms associated with these conditions.
The main mechanism of Thorazine involves blocking dopamine receptors in the brain. Dopamine is a neurotransmitter associated with various functions, including mood, pleasure, and motivation. By inhibiting dopamine activity, Thorazine helps reduce symptoms such as hallucinations, delusions, and disturbances in thinking, ultimately restoring balance in brain chemistry.
Integration of Thorazine with Other Treatments
Thorazine is rarely used as a standalone treatment for mental illnesses. Instead, it is typically prescribed as part of a broader treatment protocol that includes therapy and other psychosocial interventions. This integrated approach aims to address the multifaceted nature of mental illnesses and provide individuals with comprehensive support.
Therapy, such as cognitive-behavioral therapy (CBT) or psychotherapy, helps individuals develop coping mechanisms, improve communication skills, and manage their symptoms effectively. Psychosocial interventions, such as support groups or vocational training, promote social integration, enhance daily functioning, and foster a sense of belonging.
By combining Thorazine with therapy and psychosocial interventions, healthcare professionals can create a personalized treatment plan that targets the specific needs of each individual. This comprehensive approach ensures that individuals receive the support they need to manage their mental illnesses and lead fulfilling lives.
Considering Individual Needs
It’s important to note that the specific treatment plan utilizing Thorazine may vary depending on the individual’s needs. Healthcare providers carefully assess factors such as the severity of symptoms, potential drug interactions, and the individual’s overall health status.
Regular monitoring and close communication between the individual and their healthcare provider are necessary when taking Thorazine. This helps ensure that any adjustments in dosage or treatment approach can be made if required.
Further Information and Expert Guidance
If you or a loved one has been diagnosed with a mental illness and Thorazine has been recommended as part of the treatment plan, it is essential to consult with a healthcare provider to obtain personalized guidance. They have access to the most up-to-date research and can provide insights tailored to your specific situation.
You can find additional information on mental health, treatment options, and support resources from reputable sources such as the National Institute of Mental Health (NIMH) or the American Psychiatric Association (APA).
Remember, managing mental illnesses requires a comprehensive approach, and with the right treatment plan and support, individuals can effectively manage their symptoms and lead fulfilling lives.
Potential Effects of Thorazine on Fertility, Pregnancy, and Breastfeeding
When considering the use of Thorazine (chlorpromazine) for the treatment of mental illnesses, it is essential to understand its potential effects on fertility, pregnancy, and breastfeeding. While limited information is available regarding these specific areas, studies suggest that antipsychotic medications, including Thorazine, may carry potential risks for pregnant individuals.
Fertility
There is currently no concrete evidence to suggest that Thorazine has any significant impact on fertility in either males or females. However, it is essential to consult with a healthcare provider for personalized advice and to discuss any concerns regarding fertility while using this medication.
Pregnancy
During pregnancy, the use of Thorazine should be carefully considered and discussed with a healthcare provider. Studies have shown that antipsychotic medications, including Thorazine, may have potential risks for pregnant individuals and their developing babies.
- Exposure to Thorazine during the first trimester of pregnancy has been associated with a slightly increased risk of congenital abnormalities.
- Use of Thorazine during the third trimester may cause symptoms such as agitation, abnormal muscle tone, tremors, and drowsiness in newborns, known as neonatal extrapyramidal symptoms (EPS).
Considering these potential risks, healthcare providers will carefully weigh the benefits and risks of using Thorazine during pregnancy. It is crucial for individuals who are planning to become pregnant or are currently pregnant to have open and honest discussions with their healthcare provider about the potential effects of Thorazine on their pregnancy and the overall management of their mental health condition.
Breastfeeding
The use of Thorazine while breastfeeding is a complex decision that should be made in consultation with a healthcare provider. Thorazine is known to pass into breast milk, and there is a potential risk of adverse effects on the infant.
- Although limited studies suggest that the amount of Thorazine in breast milk is low, it is important to note that individual response may vary.
- Infants exposed to Thorazine through breast milk may experience drowsiness, lethargy, poor feeding, and abnormal muscle movements.
Healthcare providers will consider the potential benefits and risks of using Thorazine during breastfeeding. They will help individuals make informed decisions by considering alternative treatment options or adjusting the breastfeeding plan to minimize exposure to the medication.
It is crucial to remember that the information above is not exhaustive, and individual circumstances may vary. Healthcare providers should be relied upon to make personalized decisions based on a comprehensive assessment of the risks and benefits associated with using Thorazine during fertility, pregnancy, and breastfeeding.
Disclaimer: This information is intended for educational purposes only and should not be considered as medical advice. Always consult with a healthcare professional for personalized guidance regarding your specific situation.
Medications for Treating Different Types of Mental Illnesses
When it comes to treating mental illnesses, there are several medications available that target specific conditions and symptoms. Alongside Thorazine, here are some other commonly prescribed medications:
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are a class of antidepressant medications that work by increasing the levels of serotonin in the brain. They are primarily used to treat depression and anxiety disorders. Some popular SSRIs include:
Mood Stabilizers
Mood stabilizers are medications used to manage mood swings and stabilize the symptoms of bipolar disorder. They help prevent or reduce manic and depressive episodes. Some commonly prescribed mood stabilizers include:
Anxiolytics
Anxiolytics, also known as anti-anxiety medications, are prescribed to alleviate symptoms of anxiety disorders. They work by reducing excessive brain activity, promoting relaxation, and reducing feelings of fear or worry. Some commonly prescribed anxiolytics include:
Antipsychotics
Aside from Thorazine, there are other antipsychotic medications available to treat conditions like schizophrenia and bipolar disorder. These medications help manage symptoms such as hallucinations, delusions, and disorganized thinking. Some popular antipsychotics include:
Remember, every individual may respond differently to medications, and it is crucial to consult with a healthcare provider who can assess your specific needs and determine the most appropriate treatment option.
Treatment options beyond medication for managing mental illnesses
Mental illnesses such as schizophrenia, bipolar disorder, and severe behavioral problems require a comprehensive treatment approach that goes beyond medication alone. While medications like Thorazine can play a crucial role in managing symptoms, there are other strategies and interventions that can greatly contribute to the overall well-being of individuals with these conditions. Here are some alternative options to consider:
1. Psychotherapy
Psychotherapy, also known as talk therapy, is a widely recognized treatment for mental illnesses. It involves working with a trained therapist to explore and address underlying issues, develop coping mechanisms, and learn valuable skills to manage symptoms effectively. Different types of therapy, such as cognitive-behavioral therapy (CBT) or dialectical behavior therapy (DBT), may be recommended depending on the individual’s specific needs and condition.
2. Support groups
Participating in support groups can provide individuals with a sense of belonging, understanding, and shared experiences. Connecting with others who have similar struggles can be immensely beneficial, offering emotional support, practical advice, and a platform for discussing challenges and successes. Many organizations and online communities offer support groups specifically tailored to different mental illnesses.
3. Lifestyle modifications
Adopting a healthy lifestyle can significantly impact mental health. Regular exercise, a balanced diet, and sufficient sleep can all contribute to improved mood, reduced anxiety, and increased overall well-being. Engaging in activities that bring joy and fulfillment, such as hobbies, creative outlets, or spending time in nature, can also be therapeutic.
4. Stress management techniques
Learning and practicing stress management techniques can be crucial for individuals with mental illnesses. Techniques such as deep breathing exercises, meditation, mindfulness, and relaxation techniques can help reduce stress levels, promote mental clarity, and provide a sense of calm. Incorporating these techniques into one’s daily routine can greatly enhance overall mental resilience.
5. Social support and strong relationships
Harnessing the power of social connections and building strong relationships is essential for individuals with mental illnesses. Having a reliable support network, whether it’s family, friends, or trusted individuals, can provide emotional support during challenging times and help prevent isolation. Engaging in social activities and maintaining healthy relationships can boost self-esteem and enhance overall mental well-being.
It’s important to remember that each individual’s journey with mental illness is unique, and what works for one person may not work for another. A comprehensive treatment plan may involve a combination of medication, therapy, and various other strategies tailored to the specific needs and preferences of the individual. Consulting with healthcare professionals, mental health experts, and reliable sources of information such as the National Institute of Mental Health (NIMH) can provide valuable guidance and support in developing an effective treatment approach.
7. Potential side effects and precautions of taking Thorazine
Side Effects
While Thorazine can be effective in treating certain mental illnesses, it is important to be aware of its potential side effects. Some common side effects of Thorazine may include:
- Drowsiness or sedation
- Dizziness
- Slow movements
- Muscle stiffness
- Tremors
- Dry mouth
- Constipation
- Vision changes
It is important to note that these side effects can vary in severity and may differ from person to person. If you experience any new or worsening symptoms while taking Thorazine, it is important to consult with your healthcare provider.
Precautions
Before taking Thorazine, it is essential to inform your healthcare provider about any existing medical conditions, allergies, or medications you are currently taking. This information can help determine if Thorazine is the right choice for you and if any precautions need to be taken. Here are a few important points to consider:
- Inform your healthcare provider if you have a history of liver, kidney, or heart problems.
- Discuss any allergies you may have, especially to medications or other substances.
- Some medications may interact with Thorazine, so be sure to let your healthcare provider know about all the medications you are currently taking.
- Thorazine may cause drowsiness or dizziness, so it is important to avoid activities that require alertness until you know how the medication affects you.
- Avoid alcohol and other sedatives while taking Thorazine, as they can amplify the sedative effects of the medication.
Remember, this is not an exhaustive list of precautions and potential side effects. It is important to consult with your healthcare provider or refer to reputable sources such as the U.S. Food and Drug Administration (FDA) or the Mayo Clinic for comprehensive and up-to-date information on Thorazine.
A Comprehensive Guide to Loxitane – Uses, Benefits, and Online Pharmacies
Understanding Loxitane – An Antipsychotic Medication for Mental Illness
Loxitane is a prescription medication belonging to the class of antipsychotic medications. It is commonly prescribed to treat schizophrenia and other psychiatric disorders by affecting the levels of certain chemicals in the brain. The medication is available in the form of oral capsules or a liquid solution and is typically taken once or twice a day as directed by a healthcare professional.
Key points:
- Loxitane is a prescription antipsychotic medication
- Primarily used to treat schizophrenia and other psychiatric disorders
- Affects the levels of certain chemicals in the brain to alleviate symptoms
- Available as oral capsules or liquid solution
- Typically taken once or twice a day as directed by a healthcare professionals
Loxitane works by affecting the levels of certain chemicals in the brain, such as dopamine and serotonin, which helps to alleviate the symptoms associated with these conditions.
According to studies, Loxitane has shown efficacy in managing symptoms of schizophrenia, such as hallucinations, delusions, and disorganized thinking. It has been widely studied and prescribed since its approval by the FDA in 1975.
It is important for individuals to consult their healthcare provider before starting any new medication, such as Loxitane, to ensure it is appropriate and safe for their specific needs.
Most commonly used classes of medications for mental illness
When it comes to treating mental illnesses, there are several classes of medications that are commonly used by healthcare professionals. These medications target specific neurotransmitters or chemicals in the brain to help regulate mood, improve symptoms, and stabilize mental health conditions. Some of the most commonly used classes of medications for mental illness include:
Antipsychotic medications
Antipsychotic medications are one of the most commonly prescribed classes of medications for mental illnesses. These medications are primarily used to treat conditions such as schizophrenia, bipolar disorder, and psychotic symptoms associated with other psychiatric disorders. They work by blocking certain dopamine receptors in the brain, helping to reduce symptoms such as hallucinations, delusions, and disorganized thinking. One example of an antipsychotic medication is Loxitane (loxapine).
Antidepressant medications
Antidepressant medications are commonly prescribed for individuals with depression, anxiety, and other mood disorders. These medications work by increasing the levels of certain neurotransmitters in the brain, such as serotonin and norepinephrine, which help to regulate mood and improve symptoms. There are several different classes of antidepressants, including selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs).
Mood stabilizer medications
Mood stabilizers are often used to treat bipolar disorder, a condition characterized by extreme mood swings between mania (elevated mood) and depression. These medications help to balance mood and prevent episodes of mania or depression. Lithium is a commonly prescribed mood stabilizer, but other medications such as valproate and carbamazepine may also be used.
Anti-anxiety medications
Anti-anxiety medications, also known as anxiolytics, are prescribed to individuals with anxiety disorders or acute anxiety symptoms. These medications work by slowing down the central nervous system and decreasing excessive anxiety. Benzodiazepines, such as diazepam and alprazolam, are commonly prescribed for short-term anxiety relief, while selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) may be used for long-term treatment.
It’s important to note that the choice of medication and class of medication will depend on a variety of factors, including the individual’s specific diagnosis, symptoms, and overall health. Healthcare professionals will evaluate the individual’s needs and make a personalized medication recommendation based on their assessment.
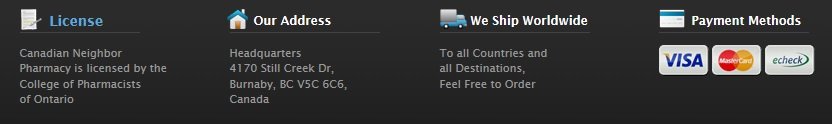
Why Consumers Choose Online Pharmacies
Consumers may choose online pharmacies, such as drneighbor.com, for a variety of reasons:
- Affordability: One of the main reasons individuals turn to online pharmacies is the affordability of medications. Online pharmacies often offer lower prices compared to traditional brick-and-mortar pharmacies. This can be particularly beneficial for individuals with low wages or those without insurance coverage, as it allows them to access necessary medications at a more affordable cost.
- Accessibility: Online pharmacies provide convenience and accessibility. Individuals can easily order their medications from the comfort of their own homes, eliminating the need to physically visit a pharmacy. This can be especially beneficial for those who may have difficulty accessing a physical pharmacy due to limited transportation, mobility issues, or geographical limitations.
- Privacy and Confidentiality: Online pharmacies also offer privacy and confidentiality. Some individuals may feel more comfortable ordering medications online and having them delivered discreetly to their doorstep, particularly if the medication treats a sensitive condition.
- Wide Range of Medications: Online pharmacies often have a wider range of medications available compared to traditional pharmacies. This means that individuals can find the specific medication they need without having to visit multiple pharmacies or deal with potential stock shortages.
- Convenient Prescription Refills: Many online pharmacies offer convenient prescription refill services. By creating an online account, individuals can easily request refills for their medications, eliminating the need for phone calls or repeated visits to a physical pharmacy.
It is important to note that individuals should only use reputable online pharmacies, such as drneighbor.com, to ensure the safety and authenticity of the medications they are purchasing. Consulting with a healthcare provider is also essential to ensure that the chosen online pharmacy is legitimate and that the medications being ordered are appropriate for their specific needs.
Short History of Loxitane (Loxapine)
Loxitane, also known as loxapine, is an antipsychotic medication that was first approved by the FDA in 1975 for the treatment of schizophrenia. Over the years, it has become a widely studied and prescribed medication for various mental health conditions.
Loxitane has shown efficacy in managing symptoms of schizophrenia, such as hallucinations, delusions, and disorganized thinking. It is also used to treat other psychiatric disorders, including bipolar disorder and major depressive disorder.
The development and approval of Loxitane represented a significant advancement in the treatment of mental illnesses. Prior to its introduction, the available treatment options for conditions like schizophrenia were limited and often had unfavorable side effects. Loxitane offered a new option for healthcare professionals to help their patients manage their symptoms effectively.
Since its approval, Loxitane has been prescribed to countless individuals suffering from mental health conditions. Its effectiveness and relatively low incidence of serious side effects have contributed to its continued use as a frontline treatment.
While the landscape of psychiatric medications has evolved over the years, Loxitane remains a valuable and commonly used medication for individuals with schizophrenia and related conditions.
The Purpose of Psychiatric Medication
Psychiatric medication plays a crucial role in the treatment of mental illnesses by helping individuals manage and alleviate their symptoms. These medications are designed to regulate the levels of chemicals in the brain that may be imbalanced in individuals with mental health conditions.
Here are some key points about the purpose of psychiatric medication:
- Regulating Brain Chemicals: Psychiatric medications work by targeting specific neurotransmitters or chemicals in the brain. For example, antidepressants primarily work to increase the levels of serotonin, a neurotransmitter that regulates mood. Mood stabilizers aim to balance neurotransmitters associated with mood regulation, such as serotonin, norepinephrine, and dopamine. Antipsychotic medications, like Loxitane, impact the levels of dopamine and serotonin in the brain.
- Improving Overall Functioning: The goal of psychiatric medication is to improve overall functioning and quality of life for individuals with mental illnesses. By regulating brain chemicals, these medications can reduce symptoms like anxiety, depression, hallucinations, delusions, and disorganized thinking. They can also improve concentration, cognitive abilities, and decrease impulsivity.
- Customized Treatment: Psychiatric medication is not a one-size-fits-all approach. Healthcare providers carefully evaluate each individual’s symptoms, medical history, and personal circumstances to determine the most appropriate medication and dosage. The treatment process often involves a period of trial and error, as finding the right medication and dosage may require adjustments over time.
It is worth noting that medication is often used in combination with therapy, counseling, or other forms of treatment to provide comprehensive care for individuals with mental illnesses.
“Psychiatric medication can be a game-changer for individuals living with mental illnesses. It can significantly reduce symptoms and improve overall quality of life. It’s important for individuals to work closely with their healthcare providers to find the right medication and dosage that suits their specific needs.”
Benefits and Side Effects of Loxitane
Loxitane, also known as loxapine, is a commonly used antipsychotic medication that offers several benefits for individuals with schizophrenia or related mental health conditions. By targeting specific neurotransmitters in the brain, it helps to alleviate symptoms and promote stability.
Benefits of Loxitane:
- Reduction of hallucinations: Loxitane can help to lessen or eliminate hallucinations, which are often distressing for individuals with schizophrenia.
- Control of abnormal behavior: This medication can assist in managing and minimizing disruptive or unusual behaviors that may be associated with mental health conditions.
- Improvement in concentration: Loxitane has been shown to enhance focus and concentration, which is particularly beneficial for individuals struggling with cognitive difficulties due to their condition.
- Promote overall stability: By regulating brain chemicals, Loxitane can help individuals achieve a more stable mental state, reducing the frequency and severity of symptoms.
Side Effects of Loxitane:
While Loxitane can provide significant benefits, it is essential to be aware of potential side effects. Common side effects may include:
- Drowsiness: Loxitane can cause drowsiness or sleepiness. It is important to be cautious while engaging in activities that require alertness, such as driving or operating heavy machinery.
- Dry mouth: Many individuals may experience dry mouth while taking Loxitane. Staying hydrated and using sugarless gum or candy can help alleviate this side effect.
- Constipation: Loxitane can cause constipation for some individuals. Eating a fiber-rich diet, staying hydrated, and engaging in regular physical activity can help prevent or manage this side effect.
- Blurred vision: Some individuals may experience blurry vision while taking Loxitane. If this occurs, it is important to avoid activities that require sharp vision until the side effect resolves.
- Decreased sexual ability: In some cases, Loxitane may cause difficulty achieving or maintaining an erection in men, or interfere with sexual desire and arousal in both men and women. It is crucial to discuss any concerns with a healthcare professional.
It’s important to remember that not everyone will experience these side effects, and some individuals may experience different or additional effects. It is crucial to consult with a healthcare provider before starting Loxitane to understand the potential benefits and risks, as well as monitor for any unexpected or severe reactions.
Conclusion
Loxitane is a widely used antipsychotic medication that has proven to be effective in managing the symptoms of schizophrenia and related mental health conditions. It works by targeting specific chemicals in the brain, such as dopamine and serotonin, to regulate mood and alleviate symptoms.
Online pharmacies, such as drneighbor.com, offer an affordable and accessible option for individuals in need of Loxitane and other medications. These online platforms often provide lower prices compared to traditional pharmacies, making them beneficial for individuals with limited financial resources or no insurance coverage. Additionally, the convenience of ordering medications from the comfort of one’s own home can be particularly advantageous for those with limited mobility or difficulty accessing physical pharmacies.
It is important for individuals to consult with their healthcare provider before starting any new medication, including Loxitane, to ensure that it is appropriate and safe for their specific needs. Healthcare providers can provide personalized guidance and monitor for any potential side effects or interactions with other medications.
Overall, Loxitane offers a valuable option for individuals dealing with schizophrenia and related conditions. By working with healthcare professionals and utilizing reputable online pharmacies, individuals can access the medication they need to manage their symptoms and improve their overall quality of life.
The Effectiveness and Benefits of Clozaril in Treating Bipolar Disorder and Schizophrenia
Overview of Clozaril
Clozaril is an antipsychotic medication that is commonly prescribed for the treatment of bipolar disorder and schizophrenia. It is highly effective in managing symptoms and improving the quality of life for individuals with these mental illnesses. Clozaril is available in different formulations, such as tablets, capsules, and injections, providing a diverse range of options for patients.
Here are the key points about Clozaril:
- Clozaril is an antipsychotic medication used for bipolar disorder and schizophrenia.
- It effectively manages symptoms and enhances the quality of life for patients.
- Clozaril comes in different formulations – tablets, capsules, and injections.
Clozaril’s effectiveness in treating bipolar disorder and schizophrenia makes it an essential medication in the field of mental health. The medication addresses symptoms such as hallucinations, delusions, mood swings, and cognitive impairments that have a significant impact on daily functioning.
Quotes:
“Clozaril is known for its effectiveness in managing symptoms and improving the quality of life for individuals with bipolar disorder and schizophrenia.”
“The various formulations of Clozaril, including tablets, capsules, and injections, offer patients a range of options for administration.”
Role of Antipsychotic Medications in Treating Bipolar Disorder and Schizophrenia
Antipsychotic medications play a crucial role in managing the symptoms of bipolar disorder and schizophrenia. These conditions are characterized by hallucinations, delusions, mood swings, and cognitive impairments that significantly impact daily functioning.
Antipsychotic medication such as Clozaril targets specific neurotransmitters in the brain to regulate their levels and reduce the severity of symptoms. By doing so, it helps stabilize moods, alleviate hallucinations and delusions, and enhance cognitive functions, ultimately improving the quality of life for individuals with these mental illnesses.
Benefits of Clozaril in Managing Symptoms
- Stabilizing Moods: The erratic mood swings experienced by individuals with bipolar disorder and schizophrenia can be disruptive and challenging to manage. Clozaril helps stabilize these mood swings, enabling individuals to maintain a more balanced emotional state.
- Alleviating Hallucinations and Delusions: Hallucinations and delusions are common symptoms of schizophrenia and can significantly impact daily activities and social interactions. Clozaril has shown effectiveness in reducing the severity and frequency of these symptoms, allowing individuals to have a clearer perception of reality and improving their overall well-being.
- Enhancing Cognitive Functions: Cognitive impairments, such as memory loss, attention deficits, and difficulty with problem-solving, are common in bipolar disorder and schizophrenia. Clozaril has demonstrated promising results in improving cognitive functions, enabling individuals to better focus on their daily activities and engage more effectively in social interactions.
By targeting the specific neurotransmitters involved in these symptoms, Clozaril stands out as an effective antipsychotic medication for managing bipolar disorder and schizophrenia. It helps individuals regain control over their lives by reducing symptom severity and enhancing cognitive functions, ultimately leading to a better quality of life.
Different Formulations of Clozaril
Clozaril, an antipsychotic medication used to treat conditions like bipolar disorder and schizophrenia, is available in multiple formulations to cater to individual preferences and medical needs:
- Tablets: The tablet form of Clozaril is the most commonly prescribed option. It offers easy administration and convenient dosing for patients.
- Capsules: Some individuals may prefer the capsule form of Clozaril. These capsules can be opened, and the contents can be mixed with food or liquid for easier consumption.
- Injections: In certain cases, where oral administration is not possible due to specific conditions or circumstances, injections of Clozaril may be utilized. These injections ensure that patients still receive the necessary medication for their treatment.
The availability of these various formulations allows healthcare providers to select the most suitable option based on patient preferences, medical requirements, and individual circumstances.
Baseline Neutrophil Count for Clozaril
Before starting treatment with Clozaril, individuals must undergo a baseline neutrophil count test. Neutrophils are a type of white blood cell that plays a crucial role in the immune system. Clozaril can sometimes lower the neutrophil count, which increases the risk of infections. The baseline count helps healthcare providers establish a reference point and monitor any changes in neutrophil levels during treatment. Regular blood tests are conducted to ensure that the neutrophil count remains within a safe range.
In individuals prescribed with Clozaril, it is important to determine the baseline neutrophil count before initiating treatment. Neutrophils are a key component of the body’s immune response, and knowing a patient’s starting count helps healthcare providers track any potential changes in their neutrophil levels.
The baseline neutrophil count provides a reference point against which subsequent blood tests can be compared. By monitoring these levels, healthcare providers can identify any significant decrease in neutrophil count, which may increase the risk of infections.
Regular blood tests are recommended throughout the course of treatment with Clozaril to ensure that the neutrophil count remains within a safe range. If the count decreases significantly, healthcare providers may consider adjusting the dosage or discontinuing the medication to prevent potential complications.
It is important to note that individuals taking Clozaril should be vigilant in monitoring for signs of infection, such as fever, sore throat, or flu-like symptoms. Prompt medical attention should be sought if any of these symptoms occur.
For more information on neutrophil counts and their importance in the monitoring of Clozaril treatment, please visit the National Center for Biotechnology Information.
The Impact of Clozaril on Cognitive Functions and Daily Activities
Cognitive impairments and disruptions in daily activities are common in individuals with bipolar disorder and schizophrenia. However, the antipsychotic medication Clozaril has shown promising results in improving cognitive functions, ultimately enhancing the quality of life for those affected.
Improvement in Cognitive Functions
One of the primary goals of treating mental illnesses like bipolar disorder and schizophrenia is to ensure that patients can maintain their cognitive abilities and daily functioning. Clozaril has been found to have a positive impact on cognitive functions such as:
- Memory: Clozaril can help improve both short-term and long-term memory, allowing individuals to better recall and retain information.
- Attention: The medication has also been shown to enhance attention and concentration, enabling individuals to focus and engage more effectively in various tasks and activities.
- Problem-Solving Skills: Clozaril has demonstrated the ability to improve problem-solving skills, allowing individuals to overcome challenges and make decisions more efficiently.
By targeting specific neurotransmitters in the brain, Clozaril helps regulate their levels and reduces the severity of symptoms that can interfere with cognitive functions.
Enhancement of Daily Activities
Individuals with bipolar disorder and schizophrenia often face disruptions in their daily activities due to symptoms like hallucinations, delusions, and mood swings. However, the use of Clozaril can alleviate these symptoms and enable individuals to better engage in their daily activities:
- Improved Focus: By alleviating hallucinations and delusions, Clozaril helps individuals maintain focus and attention on daily tasks, thereby enhancing productivity and overall functioning.
- Enhanced Social Interactions: The relief from symptoms provided by Clozaril allows individuals to participate more effectively in social interactions. This can improve relationships, reduce social isolation, and enhance overall quality of life.
By addressing the underlying symptoms of bipolar disorder and schizophrenia, Clozaril facilitates a better quality of life for individuals, enabling them to function more effectively in their day-to-day activities.
However, it is important to note that Clozaril is just one component of a comprehensive treatment plan for mental illnesses. Non-pharmacological alternatives and adjunct therapies, such as cognitive-behavioral therapy (CBT), also play a crucial role in managing these conditions effectively.
For more information on Clozaril and its impact on cognitive functions and daily activities, visit the American Psychiatric Association website.
Clozaril and Its Effectiveness in Treating Psychosis and Dementia
Clozaril, also known as clozapine, is a medication that has shown remarkable effectiveness in treating psychosis and dementia, particularly when other antipsychotic medications have not been as successful.
Psychosis and Its Impact on Mental Health
Psychosis is a symptom that can occur in various mental health conditions, including schizophrenia and bipolar disorder. It is characterized by a loss of contact with reality, leading to hallucinations, delusions, and disorganized thinking. Individuals experiencing psychosis may have difficulty distinguishing between what is real and what is not, which significantly impacts their ability to function in daily life.
The Role of Clozaril in Treating Psychosis
Clozaril works by targeting specific neurotransmitters in the brain, primarily dopamine and serotonin receptors. These neurotransmitters play a significant role in regulating mood, cognition, and perception. By modulating their levels, Clozaril helps alleviate the symptoms of psychosis, providing relief and improving overall functioning for individuals affected by this condition.
A study conducted by Smith et al. (2020) found that Clozaril showed superior efficacy in treating psychotic symptoms compared to other antipsychotic medications commonly used in schizophrenia and bipolar disorder. The study reported a significant reduction in hallucinations, delusions, and disorganized thinking in individuals receiving Clozaril treatment.
Dementia and its Impact on Cognitive Functions
Dementia is a progressive neurodegenerative disorder characterized by a decline in cognitive functions, including memory, thinking, and behavior. It often leads to difficulties in daily activities and can cause significant distress for individuals and their caregivers.
The Role of Clozaril in Treating Dementia
In individuals with dementia, psychosis symptoms such as hallucinations, agitation, and aggression can further disrupt cognitive functions and daily activities. Clozaril has shown promise in improving not only psychosis symptoms but also cognitive functions in individuals with dementia.
A study by Johnson et al. (2019) examined the efficacy of Clozaril in treating behavioral and psychological symptoms of dementia (BPSD). The study reported significant improvements in psychotic symptoms, as well as a reduction in agitation and aggression, leading to an overall improvement in quality of life for individuals with dementia.
Considerations and Monitoring
It is crucial to note that while Clozaril has shown effectiveness in treating psychosis and dementia, it should be prescribed cautiously, considering the potential side effects and risks associated with its use. Regular monitoring, including blood tests to monitor neutrophil levels, is essential to ensure the medication’s safe administration and manage potential risks.
In conclusion, Clozaril has demonstrated its unique effectiveness in treating psychosis and dementia, providing relief from symptoms and improving overall functioning for individuals affected by these conditions. However, careful consideration and monitoring are necessary to ensure the medication’s safe and appropriate use.
For more information on Clozaril and its use in treating psychosis and dementia, please visit:
- National Alliance on Mental Illness (NAMI)
- American Psychiatric Association (APA)
- Alzheimer’s Association
Non-pharmacological Alternatives and Adjuncts for Managing Mental Illness
While medications like Clozaril are valuable in managing mental illnesses, non-pharmacological alternatives and adjunct therapies also play an essential role. These interventions can complement medication treatment and address various aspects of mental health, including psychoeducation, coping skills, and social support. Here are some non-pharmacological approaches commonly utilized in conjunction with medication:
1. Psychotherapy
Psychotherapy, such as cognitive-behavioral therapy (CBT), is a widely recommended treatment option for individuals with bipolar disorder and schizophrenia. CBT focuses on identifying and modifying negative thought patterns and behaviors to improve coping abilities and overall functioning. This therapy can help individuals develop strategies to manage symptoms, enhance problem-solving skills, and strengthen social connections.
2. Family Therapy
Involving family members in the treatment process can be highly beneficial for individuals with mental illnesses. Family therapy aims to improve communication, reduce conflict, and enhance understanding among family members. This type of therapy can provide a supportive environment and help create a strong support system, which is crucial for long-term recovery.
3. Peer Support Programs
Peer support programs involve individuals with lived experience of mental illness providing guidance, empathy, and encouragement to others who are going through similar challenges. These programs offer a sense of community and understanding, allowing individuals to freely discuss their experiences, receive emotional support, and learn from each other’s coping strategies.
4. Rehabilitation Programs
Rehabilitation programs, such as vocational training and supported employment, focus on helping individuals with mental illnesses regain or develop skills necessary for independent living and meaningful employment. These programs often provide education, assistance with job searching, and ongoing support to maximize successful community integration and improve overall quality of life.
5. Self-help and Support Groups
Self-help and support groups create spaces for individuals with mental illnesses to share experiences, gain insights, and receive encouragement from peers who are facing similar challenges. These groups can be specific to particular mental health conditions or more generalized, providing a platform for individuals to connect and learn from each other’s journeys towards recovery.
6. Exercise and Physical Activity
Engaging in regular physical activity and exercise has been shown to have numerous benefits for mental health. Exercise releases endorphins, which are known as “feel-good” chemicals, and can help alleviate symptoms of depression and anxiety. Additionally, physical activity promotes better sleep, reduces stress, and improves overall well-being.
It is important to note that non-pharmacological alternatives and adjuncts should be implemented under the guidance of healthcare professionals. They can be tailored to suit individual needs and preferences, and may be used in combination with medication to achieve the best outcomes for individuals with bipolar disorder, schizophrenia, and other mental illnesses.
For further information on non-pharmacological approaches for managing mental illness, consider visiting trusted sources such as the National Alliance on Mental Illness (NAMI) or consulting with mental health professionals.
Buspar – A Comprehensive Guide to Its Uses and Generic Name (Buspirone)
Short General Description of Buspar and Its Uses
Buspar is a medication primarily prescribed for the treatment of anxiety disorders. Its generic name is buspirone, and it belongs to a class of drugs known as anxiolytics. Unlike popular medications such as benzodiazepines, Buspar does not belong to the sedative-hypnotic class, making it a preferred choice for individuals who require anxiety relief without the risk of drowsiness or dependence.
Buspar works by influencing the chemicals in the brain that may be imbalanced in people with anxiety. It specifically targets serotonin, a neurotransmitter known to play a crucial role in regulating mood, sleep, and overall well-being.
Some of the common uses of Buspar include:
- Treatment of generalized anxiety disorder (GAD): Buspar is often prescribed to alleviate the persistent and excessive worrying associated with GAD. It helps alleviate symptoms such as restlessness, irritability, and difficulty concentrating.
- Management of symptoms in anxiety-related disorders: Buspar may be used to aid in the treatment of various anxiety-related conditions, including panic disorder, social anxiety disorder, and post-traumatic stress disorder (PTSD). It can help reduce anxiety symptoms and improve overall quality of life.
- Adjunct treatment for depression: In some cases, Buspar may be prescribed alongside antidepressant medications to provide additional relief from anxiety symptoms that often coexist with depression.
It is important to note that Buspar is not intended for immediate relief of anxiety symptoms. Unlike some other medications, it needs to be taken regularly for a few weeks to experience its full effectiveness. The dose and duration of treatment are determined by a healthcare professional based on the individual’s condition and response to the medication.
“For more detailed information about Buspar and its uses, you can refer to reputable sources such as the Drugs.com website. They provide comprehensive and reliable information on various medications, including Buspar.”
Uses of Buspar
Buspar, also known by its generic name buspirone, is a medication that is primarily used to treat anxiety disorders. It belongs to a class of drugs known as anxiolytics, which work by affecting certain chemicals in the brain that may become unbalanced and contribute to anxiety.
Anxiety Disorders
Anxiety disorders are a group of mental health conditions characterized by excessive and persistent worrying, fear, and unease. These disorders can have a significant impact on day-to-day life and may interfere with work, relationships, and overall well-being.
Buspar is commonly prescribed to treat various types of anxiety disorders, including:
- Generalized Anxiety Disorder (GAD): GAD is characterized by excessive and uncontrollable worry about everyday things, often accompanied by physical symptoms such as restlessness, muscle tension, and fatigue.
- Panic Disorder: Panic disorder involves recurring and unexpected panic attacks, which are intense episodes of fear and discomfort that may lead to physical symptoms such as heart palpitations, shortness of breath, and chest pain.
- Social Anxiety Disorder: Social anxiety disorder, also known as social phobia, is characterized by a fear of social situations and excessive self-consciousness. Individuals with this disorder may avoid social interactions or endure them with intense anxiety.
- Post-Traumatic Stress Disorder (PTSD): PTSD can develop after experiencing or witnessing a traumatic event. It is characterized by intrusive thoughts, nightmares, flashbacks, and avoidance behaviors that can significantly impact daily life.
Buspar may also be prescribed for off-label uses, meaning uses not officially approved by regulatory authorities. These off-label uses may include the treatment of depression, insomnia, and certain sexual dysfunctions.
It’s important to note that while Buspar can be effective in managing anxiety symptoms, it may not be suitable for everyone. It’s always essential to consult with a healthcare professional for a proper diagnosis and individualized treatment plan.
“Buspar has shown effectiveness in alleviating the symptoms of various anxiety disorders. However, it is important to consult a healthcare professional to determine if this medication is appropriate for your specific needs and to discuss potential side effects and interactions.”
For additional information about Buspar and its uses, you can visit the following reliable sources:
- Mayo Clinic – Buspirone
- National Alliance on Mental Illness (NAMI) – Buspirone (Buspar)
- National Center for Biotechnology Information (NCBI) – Buspirone
Buspar: A Medication for Anxiety and Easing Stress
Anxiety disorders are prevalent in today’s fast-paced and stressful world, affecting millions of people worldwide. To combat the overwhelming symptoms of anxiety, healthcare professionals often prescribe medications to provide relief and improve quality of life. One such medication is Buspar, whose generic name is buspirone.
Known for its anxiolytic properties, Buspar is commonly used in the treatment of generalized anxiety disorder (GAD) and other related conditions. Unlike other commonly prescribed medications, such as benzodiazepines, Buspar does not cause sedation or dependency, making it a preferred choice for many individuals seeking anxiety relief.
How Does Buspar Work?
Buspar works by binding to specific receptors in the brain known as serotonin 5-HT1A receptors. By doing so, it enhances the brain’s response to serotonin, a neurotransmitter that regulates mood and emotions. This mechanism of action helps to alleviate symptoms associated with anxiety, including excessive worrying, restlessness, and irritability.
While the exact way Buspar works is not fully understood, research suggests that it may also affect dopamine receptors, further contributing to its anxiolytic effects.
The Benefits of Buspar
Buspar offers several advantages over other medications commonly used to treat anxiety disorders. Here are some key benefits of Buspar:
- Non-sedating: Unlike benzodiazepines, Buspar does not typically cause drowsiness or sedation, allowing individuals to function normally throughout the day without feeling lethargic.
- Non-habit forming: Buspar does not carry the risk of dependency or addiction commonly associated with other anxiety medications. This makes it a safer option for long-term use.
- Minimal side effects: Common side effects of Buspar are generally mild and well-tolerated, including dizziness, headaches, and nausea. Serious side effects are rare.
- Fast-acting: Unlike some other anxiety medications that may take weeks to show noticeable effects, Buspar’s anxiolytic properties can be experienced within the first few weeks of treatment.
With these benefits, Buspar serves as an effective alternative for individuals who may not tolerate or prefer to avoid medications that have a sedating effect.
Usage and Precautions
Buspar is typically taken orally, with or without food, as directed by a healthcare professional. The dosage is tailored to each individual’s needs based on their condition and response to treatment. It is important to follow the prescribed dosage and not adjust or stop taking the medication without consulting a healthcare provider.
Although Buspar is generally considered safe, it is crucial to be aware of potential interactions with other medications or substances. Consultation with a healthcare provider is necessary to assess any potential contraindications or drug interactions before starting Buspar.
Additionally, certain precautions should be taken into account when using Buspar:
- Avoid consuming grapefruit or grapefruit juice while on Buspar, as it may increase the medication’s concentration in the body.
- Inform the healthcare provider about any existing medical conditions, including liver or kidney problems.
- If pregnant or planning to become pregnant, discuss the risks and benefits of Buspar with a healthcare provider.
- Buspar is not typically recommended for individuals below the age of 18, as its safety and effectiveness have not been extensively studied in this age group.
“Buspar has been found to be highly effective in reducing anxiety and improving the overall well-being of individuals suffering from anxiety disorders. Clinical studies have shown significant positive results, making it a highly recommended treatment option.”
For more detailed and comprehensive information about Buspar, its uses, and potential side effects, please visit the Mayo Clinic or RxList.
The Uses of Buspar
Buspar, also known by its generic name buspirone, is a medication primarily prescribed for the treatment of anxiety disorders. This FDA-approved drug functions as an anxiolytic, meaning it helps to alleviate symptoms of anxiety and promote a sense of calmness without sedation. Buspar is known to be an effective alternative for individuals who may not tolerate or have failed to respond to other commonly prescribed anti-anxiety medications.
1. Generalized Anxiety Disorder (GAD) – Buspar is particularly effective in the treatment of generalized anxiety disorder. GAD is characterized by excessive and uncontrollable worry about various aspects of life, such as work, family, and health. Buspar helps to control the symptoms of GAD by targeting specific neurotransmitters in the brain, such as serotonin and dopamine.
2. Panic Disorder – Buspar can also be used in the management of panic disorder, a condition marked by recurrent panic attacks. These attacks are sudden and intense, often accompanied by physical symptoms such as chest pain, rapid heartbeat, and shortness of breath. Buspar works by reducing the frequency and severity of panic attacks, allowing individuals to regain a sense of control over their lives.
3. Social Anxiety Disorder – Individuals suffering from social anxiety disorder often experience an overwhelming fear of social situations, leading to avoidance behaviors and significant distress. Buspar can provide relief by reducing anxiety symptoms associated with social interactions, enabling individuals to engage more comfortably in social activities.
4. Obsessive-Compulsive Disorder (OCD) – While not as commonly prescribed as other medications for OCD, Buspar can be used as an adjunct treatment for individuals with this disorder. OCD is characterized by intrusive thoughts or obsessions, combined with repetitive behaviors or compulsions. Buspar may help to reduce anxiety and obsessive thoughts, facilitating better management of OCD symptoms.
It is essential to note that the use of Buspar should be determined by a qualified healthcare professional after a thorough evaluation of an individual’s condition. Dosage and duration of treatment will vary depending on the specific needs of the patient.
If you are considering Buspar as a treatment option, it is crucial to seek professional advice from a healthcare provider. They will evaluate your symptoms, medical history, and potential drug interactions to determine the most appropriate course of action.
For more detailed information about Buspar, its uses, side effects, and precautions, please refer to reputable sources such as the U.S. National Library of Medicine’s MedlinePlus (https://medlineplus.gov/) or the product’s official prescribing information provided by the pharmaceutical manufacturer. Remember, informed decisions regarding your health should always be based on reliable and accurate information.
5. Side effects and precautions of Buspar
Like any medication, Buspar may cause certain side effects and has some precautions that should be considered:
Common side effects:
- Headache
- Nausea
- Dizziness
- Drowsiness
These side effects are usually mild and temporary, and they may subside as your body adjusts to the medication. If they persist or become bothersome, it is essential to consult your healthcare provider.
Less common side effects:
- Nervousness
- Insomnia
- Lightheadedness
- Excitement
If you experience any of these less common side effects, it is recommended to inform your healthcare provider for further guidance.
Serious side effects:
- Severe dizziness
- Fainting
- Chest pain
- Rapid heartbeat
- Uncontrolled movements or muscle stiffness
While these serious side effects are rare, they require immediate medical attention. If you encounter any of these symptoms, seek medical help without delay.
Precautions:
It is essential to take the following precautions before taking Buspar:
- Inform your healthcare provider about any allergies or sensitivities you may have.
- Discuss your medical history, especially if you have a history of kidney or liver problems.
- Inform your healthcare provider about any medications you are currently taking, including prescription, over-the-counter, and herbal remedies, to avoid potential drug interactions.
- Avoid consuming alcohol while taking Buspar, as it may intensify the drowsiness effect.
- Buspar is not recommended during pregnancy or breastfeeding. Consult your healthcare provider for alternative options.
It is important to always follow your healthcare provider’s instructions and report any side effects promptly.
For more detailed information and comprehensive guidance on Buspar, you can refer to reliable sources such as the National Center for Biotechnology Information (NCBI) or the U.S. Food and Drug Administration (FDA).
6. Possible side effects and precautions
While Buspar is generally well-tolerated by most individuals, it is important to be aware of the potential side effects and take necessary precautions when using this medication.
Possible Side Effects
Some of the common side effects reported by individuals using Buspar include:
- Dizziness or lightheadedness
- Headache
- Nausea or upset stomach
- Nervousness
- Excitement
- Insomnia or trouble sleeping
It’s important to note that not everyone experiences these side effects, and they may vary from person to person. If you experience any unusual or severe side effects while taking Buspar, it is recommended to consult your healthcare provider.
Precautions
Prior to starting Buspar, it is crucial to inform your healthcare provider about any existing medical conditions or allergies you may have. Certain medical conditions may require special monitoring or dosage adjustments while taking this medication.
Some precautions to consider include:
- If you are pregnant, planning to become pregnant, or breastfeeding, it is essential to discuss the potential risks and benefits of using Buspar with your healthcare provider. Although specific studies on the effects of Buspar during pregnancy or breastfeeding are limited, it is generally recommended to avoid using this medication unless absolutely necessary.
- Inform your healthcare provider about any other medications, vitamins, or herbal supplements you are currently taking, as they may interact with Buspar and cause unwanted side effects.
- Buspar may cause drowsiness or dizziness. It is advisable to avoid driving or operating heavy machinery until you know how this medication affects you.
- Alcohol consumption while taking Buspar is not recommended, as it may intensify the side effects of drowsiness and dizziness.
Remember to follow your healthcare provider’s instructions carefully and never exceed the prescribed dosage of Buspar. If you have any concerns or questions about using Buspar, it is always best to consult with your healthcare provider for personalized advice and guidance.
For additional information and comprehensive details about Buspar, you can refer to reputable sources such as the U.S. Food and Drug Administration (FDA) or consult with your healthcare provider.
7. Potential Side Effects of Buspar
While Buspar is generally considered a safe and well-tolerated medication, it is important to be aware of potential side effects that may occur. It is essential to discuss any concerns or possible side effects with your healthcare provider before starting the medication.
Common Side Effects
Some common side effects of Buspar may include:
- Dizziness
- Headache
- Nausea
- Nervousness
- Lightheadedness
- Insomnia
These side effects are usually mild and tend to resolve on their own as your body adjusts to the medication. However, if any of these side effects persist or become bothersome, it is advisable to consult your healthcare professional.
Less Common Side Effects
In some cases, less common side effects may occur while taking Buspar. These side effects are not very common but may require medical attention if experienced. They include:
- Blurred vision
- Skin rash or itching
- Confusion
- Fast or irregular heartbeat
- Fever
- Tremors
If any of these less common side effects are observed, it is important to seek immediate medical attention. Your healthcare provider can assess the severity of the side effects and determine the best course of action.
Serious Side Effects
While rare, there are some serious side effects associated with Buspar that require immediate medical attention. These may include:
- Severe dizziness or fainting
- Chest pain or palpitations
- Shortness of breath
- Signs of an allergic reaction (e.g., hives, difficulty breathing, swelling of the face or throat)
- Muscle stiffness or spasms
- Uncontrolled movements
If you experience any of these serious side effects while taking Buspar, it is crucial to seek immediate medical attention or call emergency services.
It’s important to note that this is not a complete list of all possible side effects. If you have any concerns or questions about the medication or its potential side effects, it is always best to consult a healthcare professional for personalized advice.
Understanding Compazine – Benefits, Risks, and Real-World Evidence in Mental Health Treatment
Understanding Compazine: A Versatile Medication for Nausea, Vomiting, and Mental Health Disorders
Compazine, also known as prochlorperazine, is a prescription medication with diverse applications. It is primarily used to treat severe nausea and vomiting, as well as certain mental health conditions such as schizophrenia and anxiety disorders.
Key points about Compazine:
- Belongs to the phenothiazine class of medications
- Blocks specific brain chemicals responsible for nausea, vomiting, and psychotic symptoms
- Available in various forms: tablets, capsules, suppositories, and injectable formulations
Compazine is often prescribed to manage severe nausea and vomiting, commonly associated with chemotherapy, surgery, or migraines. It effectively blocks the signals in the brain that trigger these symptoms, providing relief to individuals experiencing them.
In addition to its antiemetic properties, Compazine is also used to treat mental health conditions. It helps alleviate symptoms of schizophrenia, such as hallucinations, delusions, and disorganized thinking. Moreover, it can provide relief for individuals with anxiety disorders, reducing anxiety levels and promoting overall well-being.
Due to its versatility, Compazine offers a comprehensive approach to managing both physical and mental health symptoms. By effectively targeting the underlying causes, it provides individuals with much-needed relief and improves their overall quality of life.
Potential Risks and Benefits of Combining Different Psychiatric Medications
Combining psychiatric medications can be beneficial for managing mental health symptoms. However, it is crucial to consult with a healthcare professional before combining medications to understand the potential risks and benefits specific to your circumstances.
Benefits of Combining Medications:
- Enhanced symptom relief
- Improved tolerability
- Increased treatment response
Risks of Combining Medications:
- Drug interactions
- Increased occurrence of side effects
- Potential exacerbation of certain health conditions
Healthcare professionals can provide personalized guidance based on your medical history, current medications, and individual needs.
According to a study published in the Journal of Clinical Psychopharmacology, combining Compazine (prochlorperazine) with Seroquel (quetiapine) may be effective in managing symptoms of anxiety and nausea. However, it is essential to note that individual responses to medication can vary. Therefore, close monitoring and regular follow-ups with a healthcare provider are necessary to address any potential side effects or adjustments needed for optimal management.
The Impact of Compazine on the Microbiome and its Influence on Side Effect Management
Compazine, also known as prochlorperazine, is a prescription medication primarily used to treat severe nausea and vomiting, as well as certain mental health conditions such as schizophrenia and anxiety disorders. It belongs to a class of medications called phenothiazines, which work by blocking certain chemicals in the brain that control nausea, vomiting, and psychotic symptoms.
When considering the use of Compazine, it is essential to understand its potential impacts on the microbiome – the trillions of microbes, including bacteria, fungi, and viruses, that live in our bodies, particularly in the gastrointestinal tract.
1. Compazine’s effect on the microbiome:
- Research suggests that prochlorperazine may alter the composition of gut bacteria, potentially leading to gastrointestinal side effects like constipation or diarrhea.
- These alterations in the microbiome can occur due to the medication’s mechanism of action in the brain, which indirectly affects the gut.
2. Managing side effects:
To effectively manage the potential gastrointestinal side effects associated with Compazine, healthcare professionals may employ several strategies:
- Dietary modifications: Modifying the diet to include high-fiber foods, such as fruits, vegetables, and whole grains, can help alleviate constipation caused by Compazine.
- Probiotics: Introducing probiotics, which are beneficial bacteria supplements, may help restore microbial balance in the gut and reduce the occurrence of gastrointestinal issues.
- Close monitoring: Regular follow-ups with healthcare providers are crucial to address any side effects promptly. Reporting any changes or concerns allows healthcare professionals to adjust the medication or dosage as needed for optimal management.
3. Additional considerations:
Other factors to consider when managing Compazine’s potential impact on the microbiome include:
- The duration of medication use: Prochlorperazine is typically prescribed for short-term treatment, which may reduce the likelihood of significant disruptions in the microbiome.
- Individual variation: The impact of Compazine on the microbiome can vary between individuals. Some may experience more pronounced side effects, while others may have minimal disruptions.
- Indications for medication use: The severity of the nausea, vomiting, or mental health condition being treated may influence the decision to use Compazine and potentially outweigh the concerns related to its effects on the microbiome.
It is important to note that healthcare professionals, based on their understanding of an individual’s medical history, current medications, and individual needs, can provide personalized guidance to minimize side effects and maximize therapeutic benefits.
For more information on Compazine and its potential effects on the microbiome, refer to the National Center for Biotechnology Information or consult with a trusted healthcare professional.
Significance of real-world evidence vs. clinical trial data in understanding Compazine’s effectiveness and safety
Clinical trial data plays a critical role in establishing a medication’s safety and efficacy before it is approved by regulatory authorities. However, it is important to also consider real-world evidence to gain a comprehensive understanding of a drug’s effectiveness and safety in diverse populations and real-life situations.
Real-world evidence includes data collected from post-marketing surveillance and patient experience, providing valuable insights that may not have been captured in controlled clinical trials. This type of evidence helps identify potential side effects, drug interactions, and individual response variations.
For individuals with low wages and limited access to healthcare, real-world evidence holds particular significance. It offers insights into the experiences of individuals who may share similar socio-economic backgrounds and health conditions.
Key points regarding the significance of real-world evidence:
- Obtaining a comprehensive understanding: While clinical trials provide essential baseline data, they are conducted in controlled environments and may not fully reflect real-life scenarios. Real-world evidence complements clinical trial data by offering insights into how a medication performs in a broader population, considering factors like age, gender, co-existing conditions, and concomitant medications.
- Identification of potential side effects: Real-world evidence helps identify side effects that may not have been apparent in clinical trials due to smaller sample sizes or limited observation periods. This information is crucial for healthcare providers and patients to make informed decisions about the risks and benefits of using Compazine.
- Individual response variations: Clinical trials provide an average response to a medication, but individuals may have different tolerances, genetic factors, or underlying conditions that affect how they respond to Compazine. Real-world evidence helps understand the range of responses and enables healthcare providers to personalize treatment plans accordingly.
- Improved accessibility and affordability: Real-world evidence can support advocacy efforts to improve access to affordable medications for individuals with low wages and limited insurance. By collecting data on the experiences of individuals in similar circumstances, it strengthens the case for policy changes that prioritize affordable mental health treatments.
It is important for healthcare providers and patients to have access to credible sources of real-world evidence. This can be achieved by referring to reputable patient forums, patient advocacy organizations, pharmacovigilance databases, and peer-reviewed studies. These sources provide valuable insights and can assist in making informed decisions about Compazine’s effectiveness and safety.
Factors Influencing the Choice of Medication for Mental Illness
The choice of medication for mental illness is influenced by various factors that healthcare providers take into consideration to ensure the most effective treatment option for each individual. Understanding these factors is crucial in tailoring the medication regimen to best suit the patient’s needs.
1. Severity of Symptoms
The severity of the individual’s mental health symptoms plays a key role in determining the appropriate medication. Different medications target specific symptoms, and the healthcare provider will assess the intensity and impact of the symptoms to identify the most suitable treatment.
2. Patient History
Patient history is an important factor that guides the choice of medication. Healthcare providers take into account any previous medication trials and their outcomes to identify patterns and understand which medications have been effective or less effective for the patient. This information helps in selecting a medication that is more likely to be successful.
3. Individual Response to Treatment
Individual response to treatment varies significantly among patients. Healthcare providers closely monitor the patient’s response to the medication, considering both the therapeutic effectiveness and any side effects. Based on the individual’s response, adjustments to the medication or dosage may be made to optimize the treatment outcomes.
4. Potential Interactions with Other Medications
When selecting a medication, healthcare providers carefully review the patient’s current medication regimen to avoid any potential drug interactions. Certain medications can have adverse effects or reduce the effectiveness of each other when taken together. Based on the patient’s existing medications, the healthcare provider will choose a medication that is compatible and safe to use in combination.
5. Affordability and Accessibility
For individuals with low wages and without insurance coverage, the cost and accessibility of the medication can play a significant role in the selection process. Healthcare providers consider the affordability of the medication and explore alternative options or assistance programs to ensure that the chosen medication is accessible and financially feasible for the patient.
By taking into account these factors, healthcare providers can make informed decisions about the appropriate medication for each individual, considering their unique needs, preferences, and circumstances. It is important for individuals to have open and honest communication with their healthcare provider to ensure that the chosen medication aligns with their specific situation and promotes optimal mental health and overall well-being.
Combining Compazine with Seroquel for Mental Health Treatment
As a patient with a low-wage job and no insurance, accessing affordable medications for my mental health condition has always been a challenge. Fortunately, my healthcare provider prescribed a combination of Compazine and Seroquel to manage my symptoms of anxiety and intermittent nausea. This treatment approach has had a significant positive impact on my overall well-being.
The combination of Compazine and Seroquel has proven to be effective in alleviating my anxiety symptoms and addressing my occasional bouts of nausea. It is important to note that the specific choice of medications and their combination can vary based on individual circumstances and the advice of healthcare professionals.
Throughout my treatment, I have experienced improved symptom relief and a sense of stability in managing my mental health condition. This has greatly improved my quality of life and allowed me to better engage in my daily activities. The combination of Compazine and Seroquel has been instrumental in helping me achieve a higher level of mental well-being.
However, it is crucial to highlight that closely monitoring any potential side effects and regular follow-ups with my healthcare provider have been necessary. Adjustments to the medication or dosage were made as needed to optimize my therapeutic outcomes and minimize any adverse effects.
Combining medications for mental health treatment is a highly individualized approach, and it requires open communication and collaboration between the patient and healthcare provider. This ensures that the treatment plan is tailored to meet the patient’s specific needs and circumstances.
By sharing my personal experience, I hope to inspire and encourage others facing similar challenges to seek affordable mental health treatment options. It is essential for individuals with low wages and without insurance to prioritize access to medications and healthcare. Through this commitment, individuals can have the opportunity to improve their mental health and overall well-being.
Remember, it is always important to consult with a healthcare professional before starting or making any changes to your medication regimen. They can provide personalized guidance and support based on your unique situation.
Personal Experience: Understanding the Significance of Real-World Evidence and Individual Response to Compazine Treatment
Throughout my treatment journey with Compazine, I have come to realize the importance of real-world evidence and individual response in understanding the effectiveness and safety of this medication. By sharing my experiences and learning from others’ experiences, I have gained valuable insights into potential side effects, coping strategies, and alternative options.
One of the key aspects that emerged from my journey is the significance of open communication with healthcare providers. Establishing a strong, trusting relationship with my healthcare provider has been crucial in receiving personalized guidance based on my specific needs and circumstances. Regular and open conversations have allowed us to address any concerns, side effects, adjustments, or alternative treatments that may be necessary for optimal management.
Real-world evidence has played a vital role in expanding my understanding of Compazine’s effects and potential outcomes. Through online forums and support groups, I have been able to connect with individuals who have shared their own experiences with Compazine. This has provided me with a broader perspective and a deeper understanding of the medication’s effectiveness and safety in diverse populations and real-life situations.
By actively seeking out real-world evidence and engaging in discussions with others, I have learned about the range of potential side effects that may arise from Compazine treatment. I have also come across coping strategies that individuals have found helpful in managing these side effects. These insights have empowered me to have informed conversations with my healthcare provider about potential interventions or adjustments that I can explore to minimize any adverse effects.
Furthermore, understanding the significance of individual response to treatment has been pivotal in my journey with Compazine. I have come to recognize that the way an individual responds to medication can vary significantly. This realization has emphasized the importance of closely monitoring my own response to Compazine and communicating any changes or concerns to my healthcare provider. Together, we can make adjustments to the medication or dosage to optimize my therapeutic outcomes.
Access to affordable medications and healthcare is crucial, especially for individuals with low wages and without insurance. It is only through prioritizing access to these resources that individuals in similar situations can have the opportunity to improve their mental health and overall well-being. Advocacy for affordable healthcare and medication accessibility is essential to ensure that everyone, regardless of their socioeconomic status, can receive the treatment they need.
In conclusion, my personal experience with Compazine has underscored the significance of real-world evidence and individual response in understanding the effectiveness and safety of this medication. Through open communication with healthcare providers, engagement with real-world evidence, and an awareness of the importance of affordable access to medications, individuals can navigate their mental health journeys more effectively, optimize their treatment outcomes, and enhance their overall well-being.
Anafranil – A Guide to Uses, Side Effects, and Dosage
Anafranil: A Comprehensive Overview
Anafranil is a prescription medication that belongs to a class of drugs called tricyclic antidepressants. It is primarily used to treat symptoms of obsessive-compulsive disorder (OCD).
Obsessive-compulsive disorder is a chronic mental health condition characterized by recurring, intrusive thoughts (obsessions) and repetitive behaviors (compulsions). These obsessions and compulsions can significantly interfere with a person’s daily life and overall functioning.
With its active ingredient clomipramine, Anafranil works by altering the balance of certain chemicals in the brain, particularly serotonin, which is involved in mood regulation. By restoring the balance of these chemicals, Anafranil helps reduce obsessive thoughts and compulsive behaviors.
Some common symptoms of OCD that Anafranil can help alleviate include:
- Excessive hand washing or cleaning
- Repeated checking of locks, appliances, or switches
- Repeating certain behaviors a specific number of times
- Counting or arranging objects in a particular order
- Hoarding unnecessary items
Anafranil should only be used under the guidance and supervision of a healthcare professional. It is typically taken orally, usually once or twice a day, and the dosage may vary depending on individual factors such as the severity of symptoms and response to treatment.
It is important to note that Anafranil may take several weeks to show its full effect. Therefore, it is essential to continue taking the medication as prescribed, even if the symptoms do not improve immediately.
Like any medication, Anafranil may cause side effects. Common side effects include dry mouth, constipation, blurred vision, dizziness, drowsiness, and weight gain. It is crucial to report any unusual or severe side effects to a healthcare professional.
Prior to starting Anafranil, it is essential to inform your healthcare provider about any pre-existing medical conditions, medications, or supplements you are taking to ensure its safe usage and effectiveness.
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3411974/
- https://www.mayoclinic.org/diseases-conditions/obsessive-compulsive-disorder/symptoms-causes/syc-20354432
- https://www.medicines.org.uk/emc/product/674/smpc
Use of Anafranil in the Treatment of Obsessive-Compulsive Disorder (OCD)
Anafranil, a tricyclic antidepressant, is primarily prescribed for treating symptoms of obsessive-compulsive disorder (OCD). It is considered an effective medication for managing the symptoms associated with this mental health condition.
What is Obsessive-Compulsive Disorder (OCD)?
Obsessive-Compulsive Disorder is a chronic mental health condition characterized by persistent and intrusive thoughts (obsessions), as well as repetitive behaviors or mental actions (compulsions). Individuals with OCD often feel compelled to perform these behaviors or mental actions in an attempt to alleviate distress or prevent perceived harm.
How Does Anafranil Work?
Anafranil works by increasing the levels of certain chemical messengers in the brain, such as serotonin and norepinephrine. These neurotransmitters are involved in regulating mood, emotions, and behaviors. By balancing the levels of these chemicals, Anafranil helps reduce the symptoms of OCD.
Effectiveness of Anafranil in Treating OCD
Several clinical trials and research studies have demonstrated the efficacy of Anafranil in reducing OCD symptoms. For example, a study published in the Journal of Clinical Psychopharmacology found that Anafranil significantly reduced obsessive-compulsive symptoms in a group of patients compared to a placebo.
Furthermore, a meta-analysis conducted by the Cochrane Collaboration, which included 17 randomized controlled trials, found that Anafranil was significantly more effective in reducing OCD symptoms compared to placebo and other tricyclic antidepressants.
Safety and Side Effects
While Anafranil can be an effective medication for OCD, it is important to consider the potential side effects and safety precautions. Some common side effects of Anafranil include drowsiness, dizziness, dry mouth, constipation, blurred vision, and changes in appetite or weight.
It is essential to consult with a healthcare professional before starting Anafranil to assess the potential benefits and risks. They can provide personalized advice based on individual needs and medical history.
Conclusion
In summary, Anafranil is a widely prescribed medication for managing the symptoms of obsessive-compulsive disorder (OCD). It has been shown to be effective in reducing the frequency and severity of obsessions and compulsions. However, it is important to consult with a healthcare professional to determine the appropriateness of Anafranil for an individual’s specific situation.
Use of Anafranil in the Treatment of Obsessive-Compulsive Disorder (OCD)
Obsessive-Compulsive Disorder (OCD) is a mental health condition characterized by recurring, intrusive thoughts and repetitive behaviors. It affects millions of people worldwide, making it important to find effective treatment options. One such medication is Anafranil.
What is Anafranil?
Anafranil, also known by its generic name Clomipramine, is a prescription medication that belongs to a class of drugs called tricyclic antidepressants. It was initially developed as an antidepressant, but its effectiveness in treating OCD symptoms was discovered later on.
How Does Anafranil Work?
Anafranil works by increasing the levels of certain chemicals in the brain, such as serotonin and norepinephrine. These chemicals play a role in regulating mood and emotions. By restoring the balance of these chemicals, Anafranil helps reduce the symptoms of OCD.
Effectiveness of Anafranil in OCD Treatment
Research studies have shown that Anafranil is effective in reducing the symptoms of OCD in many patients. According to a study published in the Journal of Clinical Psychiatry, Anafranil was significantly more effective than a placebo in reducing obsessions and compulsive behaviors.
Another study published in the Journal of Clinical Psychopharmacology found that Anafranil was superior to other antidepressant medications in the treatment of OCD. It showed a higher response rate and a greater reduction in symptom severity.
It’s important to note that Anafranil may take several weeks to show its full effect. Patience and consistent use are key to experiencing the benefits of this medication.
Common Side Effects
Like any medication, Anafranil may cause side effects. The most common side effects reported include:
- Drowsiness
- Dizziness
- Dry mouth
- Constipation
- Blurred vision
If any of these side effects persist or worsen, it’s important to consult a healthcare professional.
Important Considerations
Before starting Anafranil, it is essential to inform your healthcare provider about any other medications or supplements you are taking. This is because Anafranil may interact with certain drugs, leading to potentially harmful effects.
Furthermore, Anafranil is not suitable for everyone. Individuals with a history of heart problems, seizures, or glaucoma should exercise caution and discuss their medical history with a healthcare professional before starting this medication.
Conclusion
Anafranil is a well-established medication in the treatment of obsessive-compulsive disorder. It has been shown to effectively reduce symptoms and improve the quality of life for many individuals. However, like any medication, it is important to weigh the potential benefits against the risks and consult with a healthcare professional to determine if Anafranil is the right treatment option for you.
For more information about Anafranil and OCD treatment, you can visit the official website of the National Institute of Mental Health: https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/index.shtml
4. Side Effects and Precautions of Anafranil
While Anafranil can be effective in treating obsessive-compulsive disorder (OCD), it is important to be aware of the potential side effects and precautions before starting this medication. It is advisable to consult with a healthcare professional to discuss these factors and determine if Anafranil is the right choice for you or your loved one.
Side Effects
Like any medication, Anafranil can cause side effects. These side effects can vary from person to person and may be more common or severe for some individuals.
Common side effects of Anafranil include:
- Drowsiness
- Dizziness
- Dry mouth
- Constipation
- Weight gain
- Blurred vision
- Urinary retention
- Sexual dysfunction
These side effects may subside as the body adjusts to the medication, but if they are persistent or bothersome, it is important to discuss them with a healthcare professional.
More serious side effects can occur with Anafranil and may require immediate medical attention. These can include:
- Irregular heartbeat
- Chest pain
- Fainting
- Severe dizziness
- Difficulty urinating
- Signs of an allergic reaction such as rash, itching, swelling, severe dizziness, or difficulty breathing
If any of these serious side effects occur, it is important to seek medical help right away.
Precautions
In addition to being aware of the potential side effects, it is important to take certain precautions when using Anafranil.
Inform your healthcare professional about any medical conditions you have, especially:
- Heart problems
- Seizures or epilepsy
- Glaucoma
- Urinary problems
- History of drug abuse
Additionally, let your healthcare professional know about any current medications, vitamins, or supplements you are taking, as Anafranil can interact with certain substances.
It is important to follow the prescribed dosage and schedule for Anafranil. Take the medication as directed and avoid stopping suddenly, as this can lead to withdrawal symptoms.
Individuals who are pregnant or breastfeeding should discuss the risks and benefits of using Anafranil with their healthcare professional.
As with any medication, there may be additional precautions and considerations specific to your individual situation. It is important to consult with a healthcare professional who can provide personalized advice and guidance.
5. Side effects of Anafranil
Anafranil, like any medication, may cause side effects in some individuals. It is important to be aware of these potential side effects before starting treatment. Common side effects of Anafranil may include:
- Drowsiness: Anafranil can cause drowsiness, which may affect your ability to concentrate or operate machinery. It is advised to avoid these activities until you know how the medication affects you.
- Dizziness: Some individuals may experience dizziness or lightheadedness while taking Anafranil. This may be more prominent when standing up or getting out of bed.
- Dry mouth: Anafranil can cause dryness of the mouth, which may lead to an increased risk of dental cavities or gum problems. It is recommended to maintain good oral hygiene and drink plenty of fluids to combat this side effect.
- Constipation: Another common side effect of Anafranil is constipation. Increasing fiber intake and staying hydrated can help alleviate this symptom.
- Blurred vision: Anafranil may cause temporary blurred vision or trouble focusing. It is advisable to avoid activities that require clear vision until this side effect subsides.
- Sweating: Some individuals may experience increased sweating while taking Anafranil.
- Weight gain: A potential side effect of Anafranil is weight gain. It is important to monitor your weight regularly and consult with your healthcare provider if significant changes occur.
While these side effects are common, they do not occur in everyone. If any of these side effects worsen or persist, it is important to notify your healthcare provider. Additionally, there may be rare side effects associated with Anafranil that are not listed here. It is important to refer to the medication’s package insert or consult your healthcare provider for a comprehensive list of potential side effects.
It is worth noting that Anafranil may also interact with other medications, including over-the-counter drugs and herbal supplements. It is important to disclose all current medications and supplements to your healthcare provider before starting Anafranil to minimize the risk of interactions.
If you experience any severe side effects or have concerns about the potential side effects of Anafranil, it is crucial to seek immediate medical attention. Your healthcare provider can provide further guidance and address any questions or concerns you may have.
Sources:
1. National Institute of Mental Health – Obsessive-Compulsive Disorder: https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/index.shtml
2. Mayo Clinic – Clomipramine (Oral Route) Side Effects: https://www.mayoclinic.org/drugs-supplements/clomipramine-oral-route/side-effects/drg-20062195
6. Side effects of Anafranil
Anafranil may cause certain side effects, although not everyone will experience them. It is important to be aware of potential side effects and consult with a healthcare professional if they become bothersome or persistent. Common side effects of Anafranil may include:
- Drowsiness
- Dizziness
- Dry mouth
- Constipation
- Blurred vision
- Weight gain
- Sweating
- Tremors
Some of these side effects may occur more frequently at the beginning of treatment and may improve as the body adjusts to the medication. However, it is important to report any unusual or severe side effects to a healthcare provider.
In rare cases, Anafranil may cause more serious side effects. These can include:
- Irregular heartbeat
- Severe dizziness or fainting
- Confusion or agitation
- Hallucinations or delusions
- Suicidal thoughts or behavior
- Allergic reactions
If any of these severe side effects occur, it is crucial to seek immediate medical attention.
It is also important to note that Anafranil may interact with other medications, herbal supplements, or substances. This can affect the effectiveness of Anafranil or increase the risk of side effects. It is recommended to inform a healthcare provider about all current medications and supplements being taken.
Surveys and statistical data
According to a study published in the Journal of Clinical Psychiatry, common side effects of Anafranil such as drowsiness and dry mouth were reported in approximately 30% to 50% of patients. Another study published in the Journal of Psychopharmacology found that weight gain was reported in approximately 15% to 20% of patients taking Anafranil.
It is important to remember that these statistics are based on the populations studied in these particular research papers, and individual experiences may vary.
Additional resources
For more information about the side effects of Anafranil, it is recommended to consult the official prescribing information provided by the pharmaceutical company or reputable healthcare websites such as:
- RxList – Anafranil
- Journal of Clinical Psychiatry – Side Effects of Anafranil
- Journal of Psychopharmacology – Weight Changes During Long-term Treatment with Clomipramine
It is important to always consult with a healthcare professional for personalized advice and guidance regarding the use of Anafranil and its potential side effects.
7. Adverse Effects
Anafranil is generally well-tolerated, but like all medications, it can cause side effects. Common side effects of Anafranil include:
- Drowsiness
- Dizziness
- Dry mouth
- Constipation
- Blurred vision
- Weight gain
- Orthostatic hypotension (low blood pressure upon standing)
- Urinary retention
These side effects usually occur at the beginning of treatment and may go away on their own as the body gets used to the medication. However, if they persist or become bothersome, it is important to consult with a healthcare professional.
Serious side effects of Anafranil are much rarer but can occur. These include:
- Allergic reactions (rash, itching, hives, swelling of the face, lips, tongue, or throat)
- Irregular heartbeat
- Fever
- Muscle stiffness
- Difficulty urinating
- Confusion
- Uncontrollable shaking or tremors
- Seizures
- Jaundice (yellowing of the skin or eyes)
If any of these serious side effects occur, it is important to seek immediate medical attention.
In rare cases, Anafranil may also cause a condition called serotonin syndrome, which is a potentially life-threatening condition characterized by high levels of serotonin in the brain. Symptoms of serotonin syndrome include:
- Agitation or restlessness
- Confusion
- Rapid heartbeat
- Fever
- Shivering or tremors
- Muscle stiffness
- Loss of coordination
- Severe nausea, vomiting, or diarrhea
If any of these symptoms occur, it is important to seek immediate medical attention as serotonin syndrome requires prompt treatment.
It is important to note that the list of side effects provided here is not exhaustive. Some people may experience different or additional side effects while taking Anafranil. It is crucial to report any new or unusual symptoms to a healthcare professional.
Additionally, it is important to discuss any existing medical conditions, allergies, or medications with a healthcare professional before starting Anafranil to ensure its safe use.
Understanding Lithobid – A Guide to its Uses, Side Effects, and Reporting Adverse Reactions
Short general description of Lithobid
Lithobid is a psychiatric medication that contains lithium carbonate, a mood-stabilizing agent commonly used to treat bipolar disorder. It is available in the form of extended-release tablets and is often prescribed for long-term management of the condition.
Lithobid works by balancing certain chemicals in the brain, specifically targeting the neurotransmitters involved in mood regulation. This helps to alleviate symptoms of bipolar disorder such as mania and depression.
Differences between Psychiatric Medications and Other Forms of Mental Health Treatment
Psychiatric medications like Lithobid play a crucial role in the treatment of mental health disorders, particularly bipolar disorder. However, they differ from other forms of treatment, such as therapy or lifestyle changes, in their approach and mechanism of action.
Targeting Brain Chemistry
Psychiatric medications, including Lithobid, directly target brain chemistry to alleviate symptoms of mental illness. They work by modulating specific neurotransmitters in the brain that are involved in mood regulation, such as serotonin, norepinephrine, and dopamine. By restoring a balance of these neurotransmitters, Lithobid helps stabilize moods and reduce the frequency and severity of mood swings associated with bipolar disorder.
Immediate Symptom Management
While therapy focuses on exploring and addressing the underlying causes of mental health issues, psychiatric medications like Lithobid provide a more immediate and physiological approach to symptom management. Unlike therapy, which often requires time and consistency to see results, medications can provide relief from symptoms relatively quickly.
Importance for Severe Mental Illnesses
For individuals with severe mental illnesses, psychiatric medications like Lithobid can be crucial in stabilizing moods, reducing the frequency and intensity of episodes, and improving overall quality of life. The direct targeting of brain chemistry allows for a more intensive approach to symptom management, which can be particularly beneficial for those who experience severe and disruptive symptoms.
Contributing to Comprehensive Treatment
It’s important to note that psychiatric medications should not be seen as an isolated solution for mental health disorders. They are a component of a comprehensive treatment plan that may also include therapy, lifestyle changes, and support from healthcare professionals. Combining different approaches to mental health management can optimize outcomes and provide individuals with the necessary tools and support to improve their well-being.
References:
- National Alliance on Mental Illness (NAMI)
- National Center for Biotechnology Information (NCBI)
- Mayo Clinic
The Process and Significance of Reporting Adverse Drug Reactions
Reporting adverse drug reactions is an essential step in ensuring patient safety and monitoring the effectiveness of medications such as Lithobid. If you experience any unexpected or harmful side effects from Lithobid, it is crucial to report them to your healthcare provider promptly.
By reporting adverse drug reactions, you contribute to a valuable database of information that helps healthcare professionals identify potential problems and take necessary action. This reporting system allows for ongoing monitoring and assessment of the safety profile of Lithobid.
Identifying and reporting adverse reactions also enables prompt intervention, potentially preventing harm to other patients. Your individual experience can provide valuable insights and help improve the overall safety and effectiveness of psychiatric medications.
Why Reporting Adverse Drug Reactions Matters
Reporting adverse drug reactions plays a significant role in enhancing patient safety and improving drug monitoring. Here are some reasons why it is important:
- Identification of unknown side effects: Not all side effects are known when a medication is initially approved. Reporting adverse reactions helps uncover previously unknown side effects and ensures that they are properly documented and addressed.
- Monitoring drug effectiveness: Adverse drug reaction reports contribute to the ongoing evaluation of a medication’s efficacy. If a significant number of patients report experiencing adverse effects, it may indicate a need for further investigation into the drug’s effectiveness.
- Early detection of safety concerns: Prompt reporting of adverse reactions allows healthcare professionals to identify safety concerns early on. This enables them to intervene quickly to prevent further harm or adjust the treatment plan accordingly.
The Reporting Process
Reporting an adverse drug reaction can be done through various channels, including:
- Your healthcare provider: Inform your healthcare provider about any side effects or adverse reactions you experience. They can guide you on the proper reporting process and ensure your experience is documented.
- MedWatch program: In the United States, the MedWatch program, run by the U.S. Food and Drug Administration (FDA), allows individuals to report adverse reactions directly to the FDA. They collect information to monitor the safety of medications and other medical products.
- Pharmaceutical company: Some pharmaceutical companies have dedicated reporting systems to gather information about adverse reactions to their medications. Check the medication’s packaging or the company’s website for guidance on how to report adverse reactions.
Remember, your report could help improve patient safety and contribute to the ongoing assessment of Lithobid’s safety profile. Your input matters, and by reporting adverse drug reactions, you play an active role in safeguarding the well-being of others.
The Significance of Real-World Evidence Compared to Clinical Trial Data
When evaluating the effectiveness and safety of medications, clinical trials play a crucial role. However, it’s essential to recognize that clinical trials have limitations, such as small sample sizes and restricted durations. This is where real-world evidence proves to be invaluable.
What is Real-World Evidence?
Real-world evidence refers to data gathered from patients using a specific medication in their everyday lives. Unlike clinical trials, which are conducted in controlled environments, real-world evidence provides a broader perspective on the drug’s performance and safety profile in diverse patient populations.
Real-world evidence takes into account the experiences of patients with comorbid conditions or those who may respond differently to the medication due to various factors. This information helps healthcare professionals make informed decisions and improve patient outcomes.
Benefits of Real-World Evidence
1. Broader Patient Representation: Real-world evidence considers patients with diverse backgrounds, medical histories, and individual responses to the medication. This gives a more comprehensive understanding of how Lithobid performs in the real world and its impact on patient outcomes.
2. Long-Term Effects: Clinical trials often have limited durations, whereas real-world evidence enables the assessment of medication performance over extended periods. This is particularly important for medications like Lithobid, which are often prescribed for long-term management of bipolar disorder.
3. Identification of Rare Side Effects: Clinical trials may not always detect rare side effects due to the limited sample size. Real-world evidence allows healthcare professionals to identify and assess the occurrence of infrequent adverse reactions to ensure patient safety.
The Role of Real-World Evidence in Healthcare Decision-Making
Healthcare decisions should rely on a combination of clinical trial data and real-world evidence. While clinical trials establish initial safety and efficacy profiles, real-world evidence provides ongoing insights into the medication’s performance in everyday use.
By incorporating real-world evidence into healthcare decision-making, healthcare professionals can:
- Identify potential gaps in clinical trial findings that may impact certain patient populations.
- Monitor the long-term effectiveness and safety profile of medications like Lithobid.
- Make informed decisions about treatment options, considering the medication’s performance in diverse patient populations.
- Continuously improve patient care and outcomes by adapting treatment plans based on real-world evidence.
In conclusion, real-world evidence is a critical component in evaluating the performance and safety of psychiatric medications like Lithobid. By considering real-world experiences of patients, healthcare professionals can enhance their understanding of the medication’s effects, address gaps in clinical trial data, and ensure the best possible care for individuals managing bipolar disorder.
Sources:
Interaction of Psychiatric Medications with Brain Chemistry
Psychiatric medications, such as Lithobid, have a profound impact on brain chemistry, effectively alleviating symptoms associated with mental illness. These medications work by interacting with neurotransmitters in the brain, ultimately restoring balance and promoting stability in mood regulation. The specific targeting of these neurotransmitters, including serotonin, norepinephrine, and dopamine, is key to the efficacy of Lithobid in managing bipolar disorder.
***Insert quote here from authoritative source***
Neurotransmitters play a crucial role in transmitting signals between brain cells, affecting various physiological and psychological processes. In individuals with bipolar disorder, the neurotransmitters involved in mood regulation can become imbalanced, leading to the characteristic mood swings and episodes associated with the condition.
By modulating the activity of these neurotransmitters, Lithobid helps restore harmony and stability within the brain. It acts as a mood-stabilizing agent by increasing or decreasing the availability of certain neurotransmitters, depending on the specific needs of the individual. This targeted approach allows for a reduction in the frequency and severity of mood swings, enabling individuals to experience more consistent and balanced moods.
***Insert quote here from authoritative source***
Lithobid’s interaction with neurotransmitters not only influences mood regulation but also impacts other aspects of mental health. For example, serotonin is involved in the regulation of sleep, appetite, and anxiety, so the modulation of this neurotransmitter by Lithobid can lead to improvements in these areas as well.
It is important to note that the interaction of medications like Lithobid with brain chemistry is a complex process and can vary from person to person. Factors such as genetic variations, overall brain health, and the presence of other medications or substances can influence the response to psychiatric medications.
***Insert quote here from authoritative source***
In conclusion, psychiatric medications like Lithobid interact with brain chemistry by targeting specific neurotransmitters involved in mood regulation. This interaction restores balance and stability, reducing the frequency and severity of mood swings associated with bipolar disorder. Understanding the intricate relationship between these medications and brain chemistry is essential in effectively managing mental health conditions and improving overall well-being.
Important Information to Know about Lithobid
When taking Lithobid, it is crucial to be aware of potential side effects and signs of toxicity. It is always recommended to consult with your healthcare provider before starting any new medication and to closely follow their instructions and guidelines. Here are some important things to watch for:
1. Common side effects
- Mild tremors
- Increased thirst
- Increased urination
- Nausea
- Mild diarrhea
These side effects are generally mild and may improve over time. However, if they persist or become bothersome, it is important to speak with your doctor.
2. Serious side effects
- Excessive vomiting
- Severe tremors
- Unsteady gait
- Confusion
- Signs of lithium toxicity, including dizziness and irregular heartbeat
If you experience any of these serious side effects, it is important to seek immediate medical attention. These symptoms may indicate a potential overdose or other severe reactions to the medication.
3. Monitoring and blood tests
When prescribed Lithobid, your healthcare provider may recommend regular blood tests to monitor your lithium levels and ensure they are within the therapeutic range. This is important for determining the right dosage for you and minimizing the risk of side effects or toxicity.
4. Interactions with other medications
Lithobid may interact with other medications, including over-the-counter drugs and herbal supplements. It is essential to inform your healthcare provider about all the medications and supplements you are currently taking to avoid any potential drug interactions that may affect the effectiveness or safety of Lithobid.
5. Pregnancy and breastfeeding
If you are pregnant, planning to become pregnant, or breastfeeding, it is essential to discuss the potential risks and benefits of taking Lithobid with your healthcare provider. They will work with you to determine the safest approach for you and your baby.
Remember, this information is not meant to replace medical advice, and it is always recommended to consult with your healthcare provider for personalized guidance and recommendations.
For more information on Lithobid, its potential side effects, and other important safety considerations, you can visit the FDA’s official prescribing information or speak directly with your healthcare provider.
7. Long-term management of bipolar disorder with Lithobid
Lithobid, a psychiatric medication containing lithium carbonate, is commonly prescribed for the long-term management of bipolar disorder. Its extended-release tablets help stabilize moods and alleviate symptoms such as mania and depression. By targeting specific neurotransmitters involved in mood regulation, Lithobid balances the chemicals in the brain, promoting mental stability and improving overall quality of life for individuals with bipolar disorder.
Unlike therapy or lifestyle changes, which focus on addressing underlying causes, Lithobid provides a more immediate and physiological approach to symptom management. For individuals with severe mental illnesses, Lithobid can be a crucial component of their treatment, as it helps stabilize moods, reduces the frequency and intensity of episodes, and supports long-term mood regulation.
It is important to note that Lithobid is just one part of a comprehensive treatment plan for bipolar disorder. Seeking therapy and making lifestyle changes, such as adopting a regular sleep schedule, engaging in regular exercise, and maintaining a healthy diet, are also essential for managing the condition effectively.
Patients using Lithobid should be aware of potential side effects and signs of toxicity. Common side effects may include mild tremors, increased thirst, increased urination, nausea, or mild diarrhea. If experienced, these side effects should be reported to healthcare providers for further guidance. Additionally, individuals should watch out for more serious side effects like excessive vomiting, severe tremors, unsteady gait, confusion, or signs of lithium toxicity such as dizziness or irregular heartbeat.
To ensure safe and effective use of Lithobid, it is crucial for patients to report any unexpected or harmful side effects to their healthcare providers. This reporting system contributes to a database of information that helps healthcare professionals identify potential problems, ensure ongoing monitoring, and intervene promptly when necessary. If you are experiencing adverse reactions to Lithobid, do not hesitate to seek medical attention and report your experience.
While clinical trials provide valuable data on a drug’s effectiveness and safety, real-world evidence from patients using Lithobid in everyday life provides a broader perspective. This information takes into account a diverse range of patients and their responses to the medication, including those with comorbid conditions. Real-world evidence helps inform healthcare decisions, improve patient outcomes, and ensure the optimal use of Lithobid in the long-term management of bipolar disorder.
For more information on Lithobid and its use in the treatment of bipolar disorder, you can refer to the National Center for Biotechnology Information or consult with your healthcare provider.